"I didn't want my life to end without living it first."

“Growing up, I hated being different. I was afraid of people knowing I was sick. I had some friends, but I was insecure, which made me very reserved, uneasy, and afraid to be myself. I struggled to make genuine friendships. My parents were very supportive. They were always there for me and when I was hospitalized, they would take turns staying with me so that I was never alone. They were also very protective. I think I understand why - they were just looking out for me - but it sheltered me. Today, I’m pretty outgoing, friendly, personable, and social. It took time, though!
Cystic Fibrosis is an invisible disease. Because of that, people have a hard time understanding the gravity of it. No one really knows how sick you are because they can’t “see” it. When you look fine on the outside, people assume you are fine. I mean, sure, people can sometimes see when I'm out of breath, and if you lived with me you’d see that I’m coughing all the time and using oxygen. But other than that, it’s hard for people to grasp. It doesn’t bother me as much anymore, but there was a time when it was really frustrating. I felt so misunderstood. I want to help people realize just how difficult it really is.
I was diagnosed when I was 18 months old
I was very sickly as an infant and always at the pediatrician’s office. They didn’t know what was wrong with me for a while. When my parents learned I had a genetic lung condition called Cystic Fibrosis (CF), they were terrified. They had never heard of it before. It’s a life-shortening disease, because it ultimately results in lung failure. The doctors told them I’d live into my late teens or early twenties (I am 32 years old now).
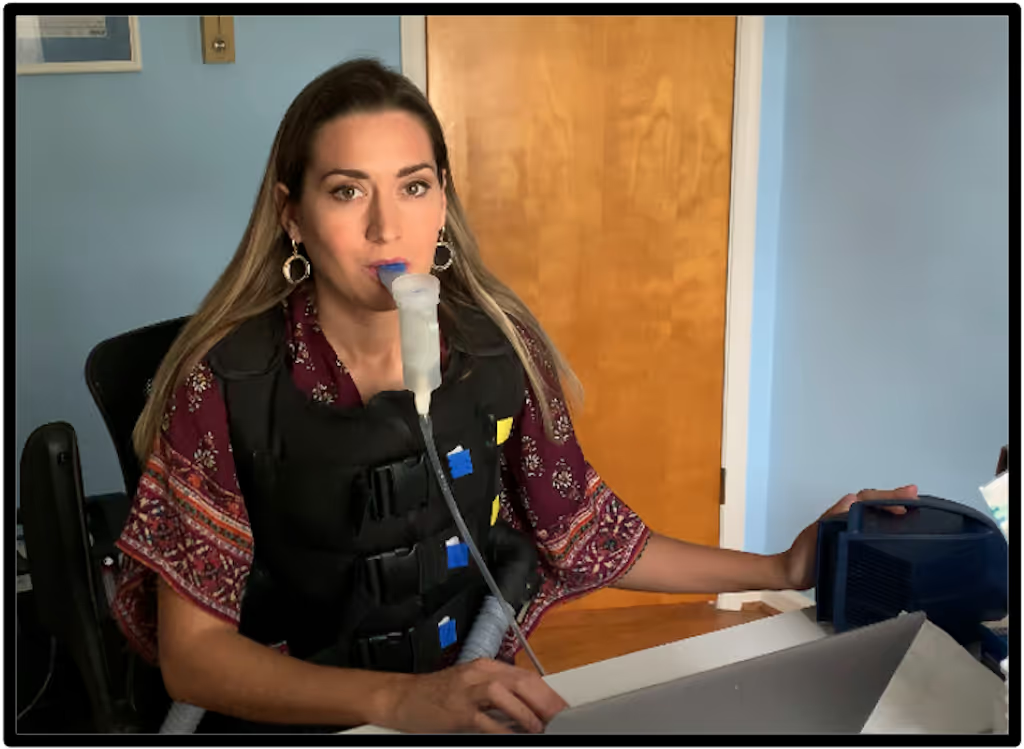
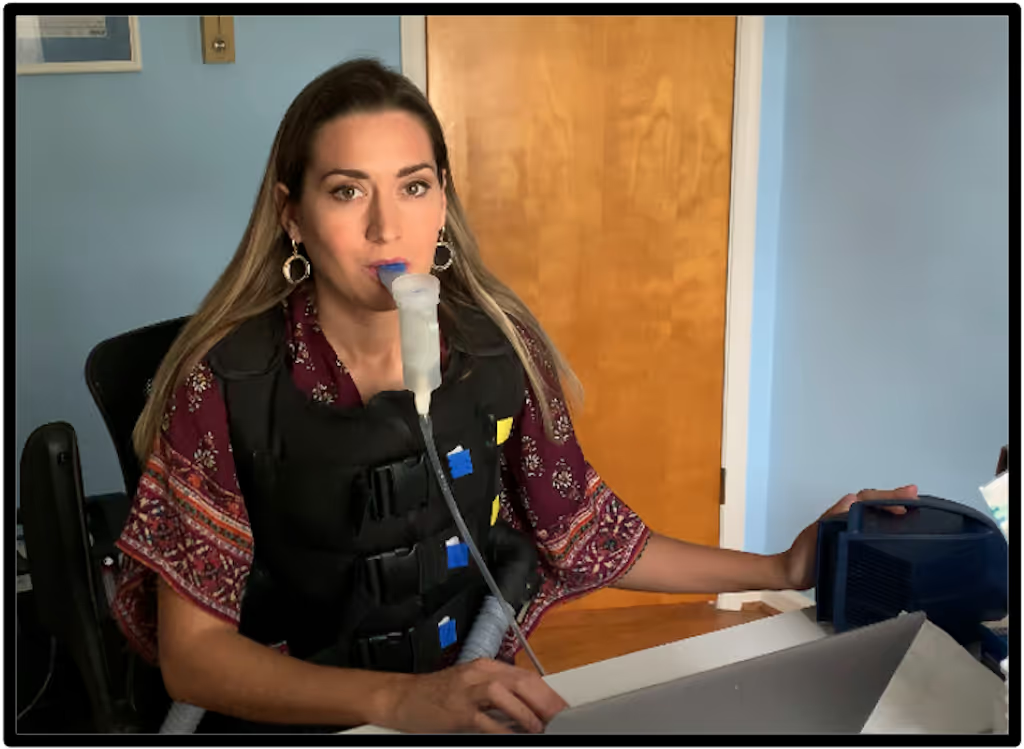
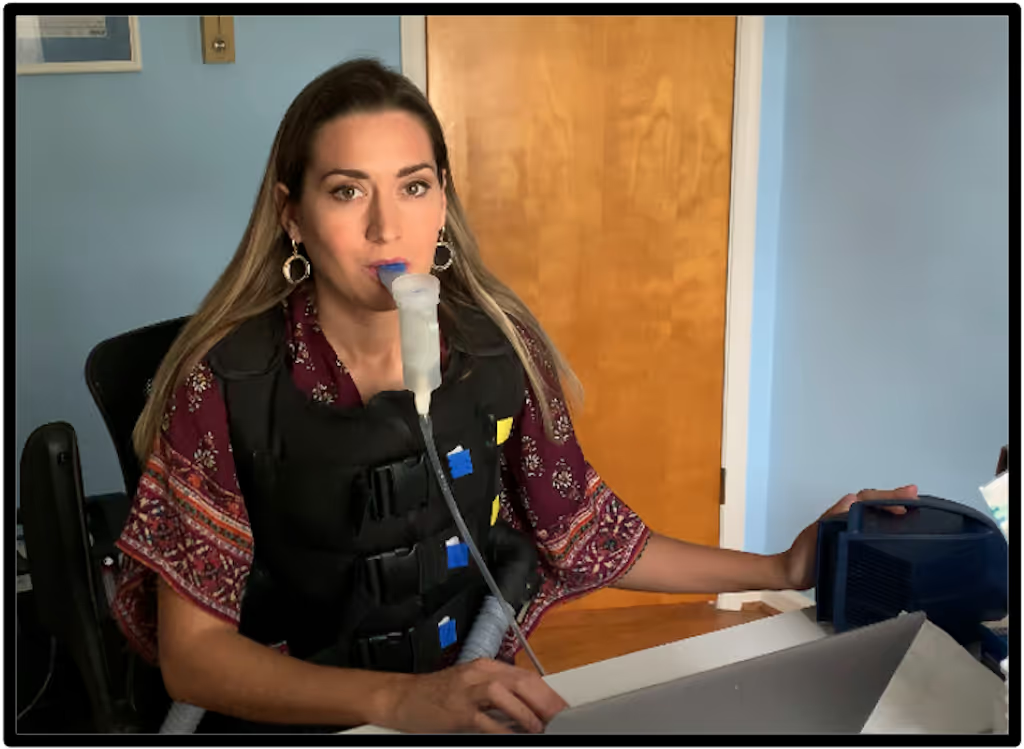
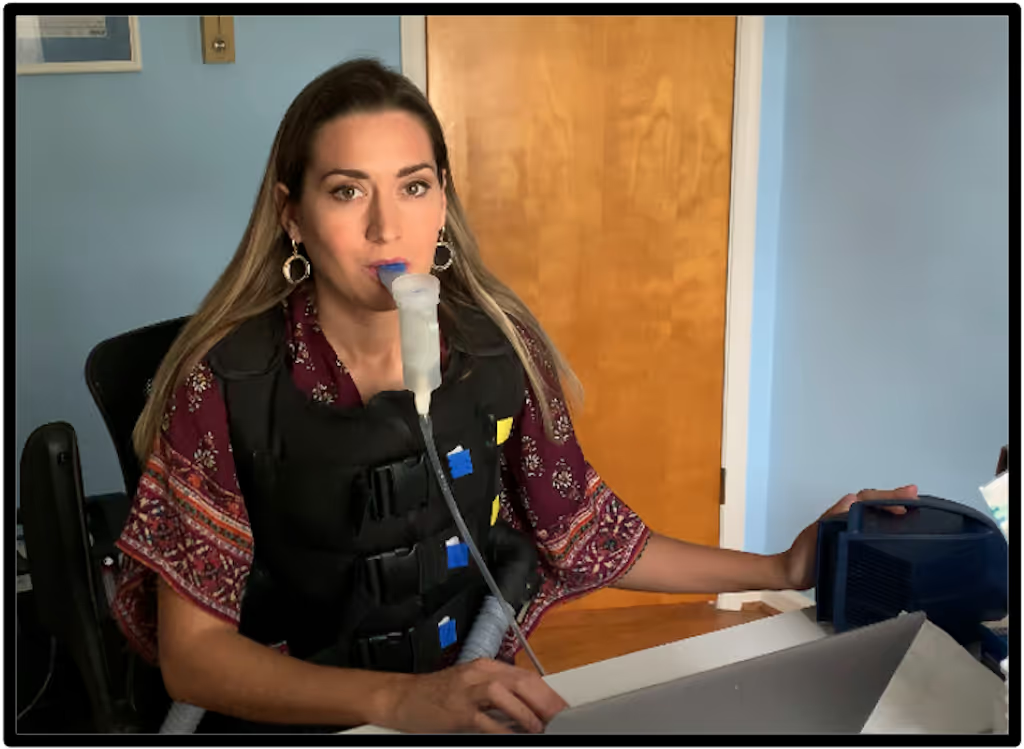
CF causes a buildup of mucus in the lungs. Three to four times a day I have to use a nebulizer with aerosolized medication to clear my airways. The treatment makes the mucus thinner so that I can cough it out, because that’s the only way to expel it. But the mucus attracts bacterial infections, which require intravenous antibiotics to treat them. I've had countless lung infections over the course of my life, so I'm very familiar with these treatments. I’d be in the hospital for three weeks at a time, multiple times a year. As I’ve gotten older, the infections have become more and more difficult to treat, because the frequent antibiotic use has led to antibiotic resistance. So there are now less antibiotics that work effectively against the bacteria. And the ones that do work take a long time to work. Most people are at 100% lung function. I’ve had less than 40% lung function for over 10 years, which is pretty low. Currently, it’s at around 28%. It’s been a slow decline.
CF is also a multi-organ-affecting disease. For most people with CF, the pancreas is also affected, which harms the production of digestive enzymes that break down food when you eat it. My pancreas doesn't produce these enzymes at all, so I have to take artificial enzyme pills when I eat. They're not as effective as our own bodies’ enzymes, so a lot of people with CF are underweight and have stomach problems. There can also be liver issues, sinus/upper respiratory issues, and CF related diabetes for some people. But not everyone is affected the same way.
I learned to accept my life exactly as it was
I went to catholic school for elementary school. It was a very small community. All the teachers knew me, so that gave me some comfort. I went to a public high school, because I wanted that experience too. But it was harsher than I expected, so I really never came out of my shell. I didn’t have many friends.
For college, I stayed local instead of going away. Part of that was my parents’ influence; they wanted to keep me close to ensure I was properly cared for by doctors. But if I’m honest, I was also scared to be on my own. So I commuted to and from school the first two years. It felt like life was “same old, same old.” I was just so unfulfilled. Eventually a shift started to happen within me, where I realized something had to change. During the spring of my sophomore year, I was really sick and in the hospital. My lungs were in bad shape and the doctors said I would likely need a transplant. It was the worst possible news. A lung transplant is a huge surgery. There’s no guarantee that it will work or that you will survive. So I had this intense moment where I knew so clearly that I didn’t want my life to end without living it first. It changed everything for me. I said to myself, “Oh my God, I might die and I haven’t lived the life that I want. Something has to change. My life has to change and only I can do that.”
Fortunately, I didn’t end up needing a transplant. But from that point on, I really started to push outside my comfort zone, whether that was meeting new people or having new experiences. I joined a sorority and started to feel more comfortable in accepting my CF diagnosis. I learned to accept my life exactly as it was and decided I was going to make the very most of it.
I err on the side of risk
In 2018, I got sick with a pretty bad infection. My lung function was at 18%. So I was taking antibiotics and on oxygen 24/7 for a couple of weeks. During that time, a company reached out to me, asking if I’d write an article for them about what it’s like to live with CF (I had started blogging prior to that, as a way to share my story and my introspective journey). They were hoping my story could accompany a short documentary they were working on. They sent me the documentary to watch, and it was all about a CF patient who was being treated at Yale with an experimental treatment called phage therapy. I had heard about phage, but didn’t know much about it. And I definitely didn’t know that someone with CF could be treated with it. Since I have a biology background, I of course started researching it and thought to myself, “I’m really, really sick and antibiotics aren’t working. They’re not a sustainable treatment option. I want to try this.”
I reached out to the researchers at Yale that day. I told them I saw the documentary and asked if they’d treat me. They got back to me really quickly. We had a long conversation about the pros and cons, and I found out there was actually minimal risk involved. They asked me to send a sample of the mucus from my lungs so they could test the bacteria, to determine the right treatment course. So I did that. I also had an appointment with my CF doctor and told him I wanted to try it. He said, “There’s no research on this. It’s not FDA approved, and it’s not even in clinical trials yet.” He was skeptical, but ultimately the decision was mine to make.
I’d say I err on the side of taking risks - maybe more so than the average person. But I was so sick and knew if I didn’t try something different, I might not live. I was certainly afraid that the treatment could make me worse and even kill me. But it was a dire situation. I was desperate. So I made the decision for myself to move forward with the phage treatment. I’m lucky that my family has always been so supportive of me. They respect and value my knowledge about my own care and trust my decision-making process. I traveled up to Yale for the treatment. My mom drove me while I laid in the back seat. The coughing and fatigue were just unbearable. It’s really scary thinking about navigating this alone. I don’t take my support system for granted!
I don’t really believe in miracles, but the serendipity of it all was truly amazing
I was treated with phage therapy for a week at Yale, but didn’t feel much different after. I came back home to Richmond and saw my CF doctor a few days later. He said, “Well, you tried it. But nothing’s changed. You’re very sick, and we should move forward with you getting a lung transplant.” There’s nowhere to get a transplant in Richmond, so I went to Duke University hospital in North Carolina. I was admitted to the hospital there getting IV antibiotics, and for some testing and prep for the transplant. But a couple days later, I started clearing out my infection. I had taken these antibiotics before but never had results like this. So I called the researchers at Yale, and we realized that the phage therapy had changed my bacterial sensitivities. The synergy of the phage and the antibiotic working together helped to kill the bacteria and subdue the acute infection. The serendipity of it all was truly amazing. If that company hadn’t reached out about writing a blog article, I wouldn’t have known about the phage treatment as an option, and likely could have been transplanted or a worse outcome that I don’t want to think about.
After I received that experimental treatment and realized it helped, my first thought was that I wanted to make other people with CF aware of it. I’ve become a big advocate for phage therapy and the development of novel therapeutics against antimicrobial resistant infections, because it’s the greatest threat to my life and anyone else living with CF. I also wanted to share my story in the hopes of inspiring others to pursue all of their options, whether that be trying an experimental treatment option, pursuing a different care option they hadn’t yet considered, or fighting their insurance company to approve a drug that could help them. I want people to take ownership of their care and push the boundaries, to see what they can achieve and if they can improve their health outcomes. I wrote an article about this and tried to get it published all over. Eventually HuffPost picked it up!
If I let my emotions take control of my mind, I’ll fall apart
Returning to what happened after the phage treatment and infection: because my body was very weak and I still had very low lung function, I decided to continue the evaluation process for transplant. But as luck would have it, a few months later as I was to be listed on the waitlist for getting new lungs, a drug was approved to treat the underlying cause of CF. So I started that drug and it stabilized me, reducing the mucus and bacterial burden in my lungs. I didn’t need the transplant as imminently anymore. The treatment doesn’t cure CF, but it slows its progression. I’ve had less infections since then and haven’t needed IV antibiotics in these last four years. It’s amazing. I still use inhaled and oral antibiotics every few months to treat lingering symptoms, I still do breathing treatments a few times a day, and I still use oxygen when I exercise and sleep. I certainly have pushed my body and do as much as I can within the limits that I have. Sometimes when I’m winded and there's a flight of stairs, I think to myself, “Ok, let’s do this.” Sometimes I can, sometimes I can’t. But my mind always wants to try.
Eventually I know my body is going to say to me, “That’s it, we have nothing left to give.” But until then, I keep pushing. It might be a coping mechanism, because if I let my emotions take control of my mind, I’ll fall apart. So I keep it moving. I just have this grit to survive. When I’ve had periods of doom - like in 2019 when I was out of breath just putting my hands over my head to wash my hair in the shower - I relied on grit. I’d focus on making it just one more hour, one more day.

I am surprised by how far I’ve made it
And I don’t mean the length of the time that I’ve lived, but rather what I’ve accomplished. I am not someone who brags about themselves or the amazing things they’ve done in their life. That’s not me. But if I really think about it from a purely factual, objective way - in terms of the impact I’ve had on the rare disease community - it’s pretty big. I’ve been flown around different cities and countries to share my story at conferences. I’ll admit, I’m always striving for that next thing, always wanting to do more to help others. So I try to remember to take a step back and be proud of what I’ve already done and the positive impact I’ve had on other people’s lives. Speaking gigs, where I talk in front of thousands of people, are really amazing (I used to get scared speaking in front of my classmates!) but I’ve realized it’s those smaller moments of connection - where I meet with people from the audience - that feel most impactful.
Over the years, I’ve made countless connections with people that reached out to me from seeing my content. The Associated Press included me in a documentary with various people experiencing lung infections (some CF related, some not). They wanted to learn about phage treatment. I connected with a lot of people during that time and was so happy to provide that kind of support and guidance. I was also part of a documentary called Silent Pandemic, where they chronicled journeys of people living with antimicrobial resistance (AMR). As mentioned, the bacteria in my lungs form resistance to the antibiotics. It’s been shared globally and has had a huge impact because of the sheer volume of people that have seen it. Hopefully it will bring more awareness to AMR and at some point down the line, inspire new research.
Another memorable connection I made was at the National Cystic Fibrosis Conference. I was walking around the exhibit hall where they had different research posters. I found a researcher who was working on phage therapy. I put two and two together and realized that the phage he was researching was the one I had taken. So I said to him, “I received a phage! The names of these look familiar to me. I’m a patient.” He was blown away. He said, “Oh my gosh, I have worked with your bacteria samples. I tested them!” He’s been doing this work for years and years in the lab, but never had the chance to actually meet a patient he had sampled. It was a really impactful moment for us both.

I’m making up for those early years
When I reflect back on all those years where I didn’t want to talk about my CF, I think it was because I was afraid of people’s judgment. But the less I care about what others think, the more I realize that most people are genuinely just curious. If given the opportunity to get to know you, they really do listen and care. That’s changed my perspective and made me more open to sharing with other people. I think there’s always an element of fear whenever you share something about yourself, but the more I’ve done it, the easier it’s become.
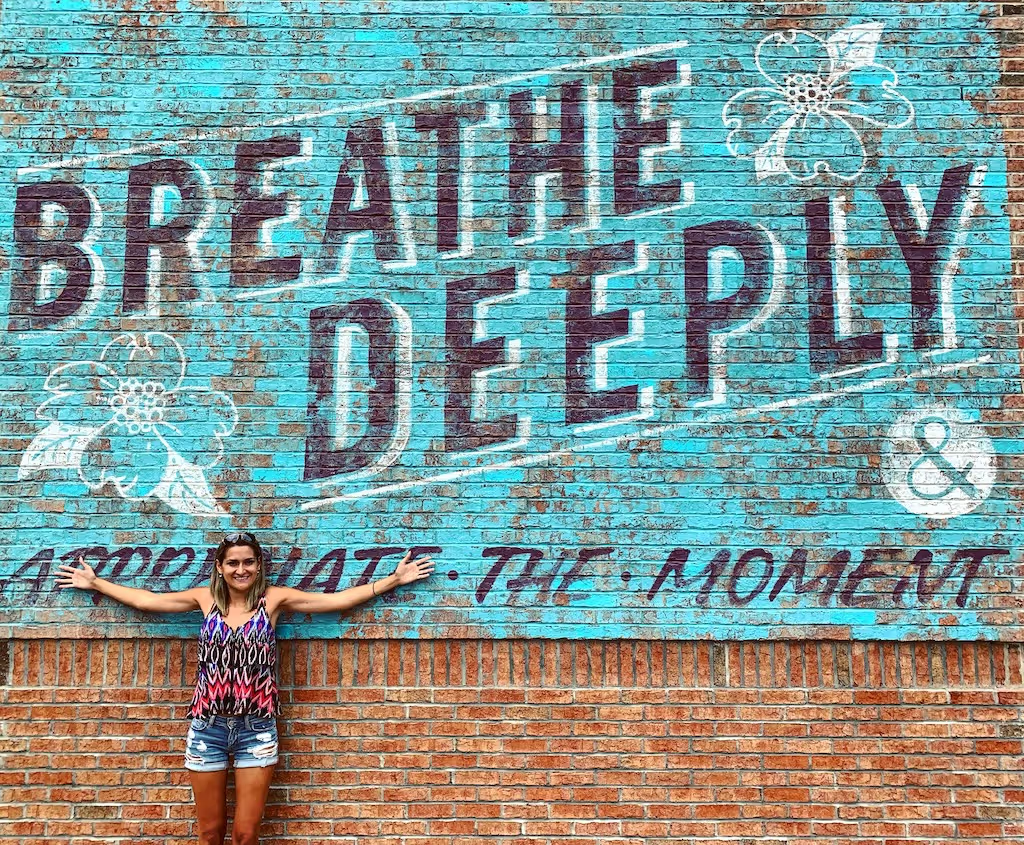
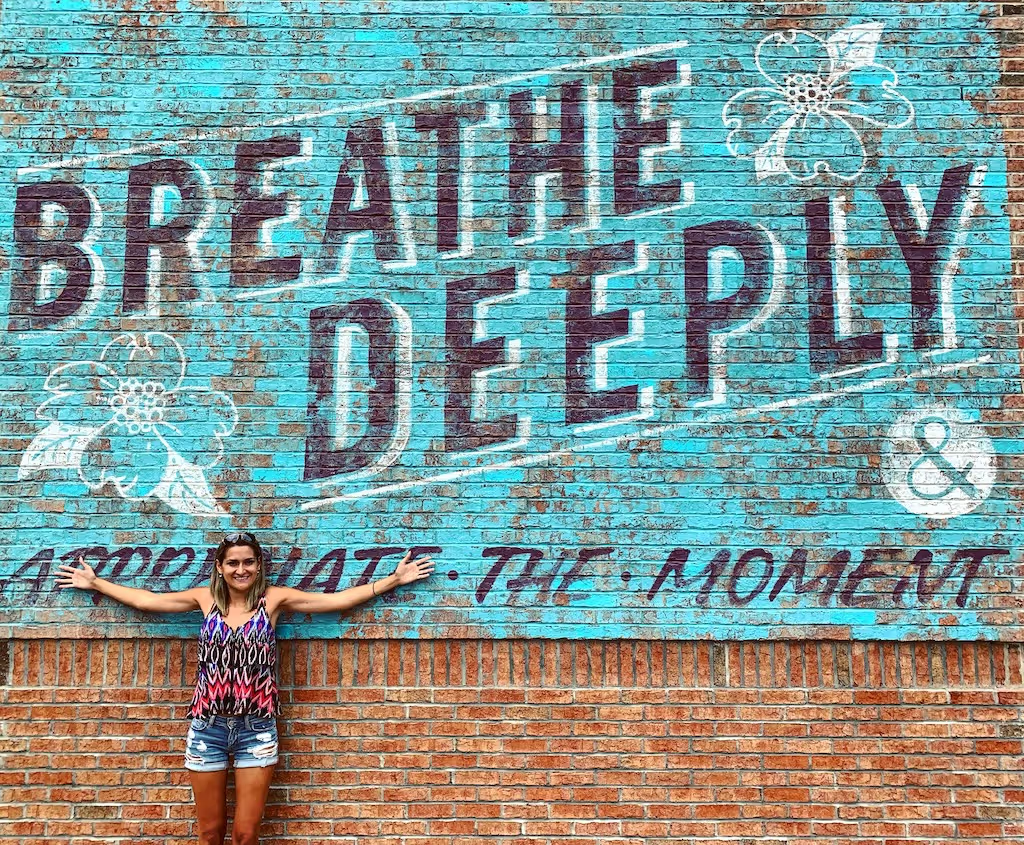
My advocacy work has always kept me really occupied, especially now that my health is more stabilized. I don’t like to wallow or dwell on things; I’ve found that there’s no use in that. If I am going to make the most of this life, I’m going to focus on the things I can control and try to let go of the rest. It’s really helped me become more social. I now have large networks both professionally and socially with friends. I’ve traveled a lot. I’ve done a lot of things. I guess in a way I’m making up for those early years. That’s maybe the catalyst for how I show up in the world now. I also just love new experiences and adventures. I like excitement! I really care about living my life to the fullest because I don’t know what things look like for me long-term. I work really hard to take care of my health as best as I can, and I stay very tuned in to the care I receive.
Writing is incredibly meaningful and cathartic for me. But I’ll admit, I’m not always consistent with it! There have been times - especially in 2018 - when my health had to be in the forefront of my mind. Every hour of every day I was struggling to live because of infections. So I didn’t write as much. But even now, despite the fact that my health has taken more of a backseat, my writing has still gotten away from me. I haven’t done as much introspection and sharing. Sometimes I’ll say to myself, “Have you turned cold? Why are you not inspired to write or share your feelings?” But I think it’s because I’m more concerned with other day-to-day things like working with new companies, being on new advisory boards, traveling for conferences, and meeting people in the rare disease community. It’s become my passion.
Cystic fibrosis has been my greatest curse and my greatest blessing. I’ve dealt with a lot of very difficult health obstacles and challenges in various ways. But I wouldn’t have gained the resilience and perspective I now have without it. I’d be more caught up in the insignificant things in life that really don’t matter, and might not be striving to live my life to the fullest as I am now. My experiences have taught me who I am and how to live my life. I wouldn’t change it.”
.avif)
To learn more about Ella’s journey and advocacy, visit her website here: https://www.ellabalasa.com/
“Growing up, I hated being different. I was afraid of people knowing I was sick. I had some friends, but I was insecure, which made me very reserved, uneasy, and afraid to be myself. I struggled to make genuine friendships. My parents were very supportive. They were always there for me and when I was hospitalized, they would take turns staying with me so that I was never alone. They were also very protective. I think I understand why - they were just looking out for me - but it sheltered me. Today, I’m pretty outgoing, friendly, personable, and social. It took time, though!
Cystic Fibrosis is an invisible disease. Because of that, people have a hard time understanding the gravity of it. No one really knows how sick you are because they can’t “see” it. When you look fine on the outside, people assume you are fine. I mean, sure, people can sometimes see when I'm out of breath, and if you lived with me you’d see that I’m coughing all the time and using oxygen. But other than that, it’s hard for people to grasp. It doesn’t bother me as much anymore, but there was a time when it was really frustrating. I felt so misunderstood. I want to help people realize just how difficult it really is.
I was diagnosed when I was 18 months old
I was very sickly as an infant and always at the pediatrician’s office. They didn’t know what was wrong with me for a while. When my parents learned I had a genetic lung condition called Cystic Fibrosis (CF), they were terrified. They had never heard of it before. It’s a life-shortening disease, because it ultimately results in lung failure. The doctors told them I’d live into my late teens or early twenties (I am 32 years old now).
CF causes a buildup of mucus in the lungs. Three to four times a day I have to use a nebulizer with aerosolized medication to clear my airways. The treatment makes the mucus thinner so that I can cough it out, because that’s the only way to expel it. But the mucus attracts bacterial infections, which require intravenous antibiotics to treat them. I've had countless lung infections over the course of my life, so I'm very familiar with these treatments. I’d be in the hospital for three weeks at a time, multiple times a year. As I’ve gotten older, the infections have become more and more difficult to treat, because the frequent antibiotic use has led to antibiotic resistance. So there are now less antibiotics that work effectively against the bacteria. And the ones that do work take a long time to work. Most people are at 100% lung function. I’ve had less than 40% lung function for over 10 years, which is pretty low. Currently, it’s at around 28%. It’s been a slow decline.
CF is also a multi-organ-affecting disease. For most people with CF, the pancreas is also affected, which harms the production of digestive enzymes that break down food when you eat it. My pancreas doesn't produce these enzymes at all, so I have to take artificial enzyme pills when I eat. They're not as effective as our own bodies’ enzymes, so a lot of people with CF are underweight and have stomach problems. There can also be liver issues, sinus/upper respiratory issues, and CF related diabetes for some people. But not everyone is affected the same way.
I learned to accept my life exactly as it was
I went to catholic school for elementary school. It was a very small community. All the teachers knew me, so that gave me some comfort. I went to a public high school, because I wanted that experience too. But it was harsher than I expected, so I really never came out of my shell. I didn’t have many friends.
For college, I stayed local instead of going away. Part of that was my parents’ influence; they wanted to keep me close to ensure I was properly cared for by doctors. But if I’m honest, I was also scared to be on my own. So I commuted to and from school the first two years. It felt like life was “same old, same old.” I was just so unfulfilled. Eventually a shift started to happen within me, where I realized something had to change. During the spring of my sophomore year, I was really sick and in the hospital. My lungs were in bad shape and the doctors said I would likely need a transplant. It was the worst possible news. A lung transplant is a huge surgery. There’s no guarantee that it will work or that you will survive. So I had this intense moment where I knew so clearly that I didn’t want my life to end without living it first. It changed everything for me. I said to myself, “Oh my God, I might die and I haven’t lived the life that I want. Something has to change. My life has to change and only I can do that.”
Fortunately, I didn’t end up needing a transplant. But from that point on, I really started to push outside my comfort zone, whether that was meeting new people or having new experiences. I joined a sorority and started to feel more comfortable in accepting my CF diagnosis. I learned to accept my life exactly as it was and decided I was going to make the very most of it.
I err on the side of risk
In 2018, I got sick with a pretty bad infection. My lung function was at 18%. So I was taking antibiotics and on oxygen 24/7 for a couple of weeks. During that time, a company reached out to me, asking if I’d write an article for them about what it’s like to live with CF (I had started blogging prior to that, as a way to share my story and my introspective journey). They were hoping my story could accompany a short documentary they were working on. They sent me the documentary to watch, and it was all about a CF patient who was being treated at Yale with an experimental treatment called phage therapy. I had heard about phage, but didn’t know much about it. And I definitely didn’t know that someone with CF could be treated with it. Since I have a biology background, I of course started researching it and thought to myself, “I’m really, really sick and antibiotics aren’t working. They’re not a sustainable treatment option. I want to try this.”
I reached out to the researchers at Yale that day. I told them I saw the documentary and asked if they’d treat me. They got back to me really quickly. We had a long conversation about the pros and cons, and I found out there was actually minimal risk involved. They asked me to send a sample of the mucus from my lungs so they could test the bacteria, to determine the right treatment course. So I did that. I also had an appointment with my CF doctor and told him I wanted to try it. He said, “There’s no research on this. It’s not FDA approved, and it’s not even in clinical trials yet.” He was skeptical, but ultimately the decision was mine to make.
I’d say I err on the side of taking risks - maybe more so than the average person. But I was so sick and knew if I didn’t try something different, I might not live. I was certainly afraid that the treatment could make me worse and even kill me. But it was a dire situation. I was desperate. So I made the decision for myself to move forward with the phage treatment. I’m lucky that my family has always been so supportive of me. They respect and value my knowledge about my own care and trust my decision-making process. I traveled up to Yale for the treatment. My mom drove me while I laid in the back seat. The coughing and fatigue were just unbearable. It’s really scary thinking about navigating this alone. I don’t take my support system for granted!
I don’t really believe in miracles, but the serendipity of it all was truly amazing
I was treated with phage therapy for a week at Yale, but didn’t feel much different after. I came back home to Richmond and saw my CF doctor a few days later. He said, “Well, you tried it. But nothing’s changed. You’re very sick, and we should move forward with you getting a lung transplant.” There’s nowhere to get a transplant in Richmond, so I went to Duke University hospital in North Carolina. I was admitted to the hospital there getting IV antibiotics, and for some testing and prep for the transplant. But a couple days later, I started clearing out my infection. I had taken these antibiotics before but never had results like this. So I called the researchers at Yale, and we realized that the phage therapy had changed my bacterial sensitivities. The synergy of the phage and the antibiotic working together helped to kill the bacteria and subdue the acute infection. The serendipity of it all was truly amazing. If that company hadn’t reached out about writing a blog article, I wouldn’t have known about the phage treatment as an option, and likely could have been transplanted or a worse outcome that I don’t want to think about.
After I received that experimental treatment and realized it helped, my first thought was that I wanted to make other people with CF aware of it. I’ve become a big advocate for phage therapy and the development of novel therapeutics against antimicrobial resistant infections, because it’s the greatest threat to my life and anyone else living with CF. I also wanted to share my story in the hopes of inspiring others to pursue all of their options, whether that be trying an experimental treatment option, pursuing a different care option they hadn’t yet considered, or fighting their insurance company to approve a drug that could help them. I want people to take ownership of their care and push the boundaries, to see what they can achieve and if they can improve their health outcomes. I wrote an article about this and tried to get it published all over. Eventually HuffPost picked it up!
If I let my emotions take control of my mind, I’ll fall apart
Returning to what happened after the phage treatment and infection: because my body was very weak and I still had very low lung function, I decided to continue the evaluation process for transplant. But as luck would have it, a few months later as I was to be listed on the waitlist for getting new lungs, a drug was approved to treat the underlying cause of CF. So I started that drug and it stabilized me, reducing the mucus and bacterial burden in my lungs. I didn’t need the transplant as imminently anymore. The treatment doesn’t cure CF, but it slows its progression. I’ve had less infections since then and haven’t needed IV antibiotics in these last four years. It’s amazing. I still use inhaled and oral antibiotics every few months to treat lingering symptoms, I still do breathing treatments a few times a day, and I still use oxygen when I exercise and sleep. I certainly have pushed my body and do as much as I can within the limits that I have. Sometimes when I’m winded and there's a flight of stairs, I think to myself, “Ok, let’s do this.” Sometimes I can, sometimes I can’t. But my mind always wants to try.
Eventually I know my body is going to say to me, “That’s it, we have nothing left to give.” But until then, I keep pushing. It might be a coping mechanism, because if I let my emotions take control of my mind, I’ll fall apart. So I keep it moving. I just have this grit to survive. When I’ve had periods of doom - like in 2019 when I was out of breath just putting my hands over my head to wash my hair in the shower - I relied on grit. I’d focus on making it just one more hour, one more day.

I am surprised by how far I’ve made it
And I don’t mean the length of the time that I’ve lived, but rather what I’ve accomplished. I am not someone who brags about themselves or the amazing things they’ve done in their life. That’s not me. But if I really think about it from a purely factual, objective way - in terms of the impact I’ve had on the rare disease community - it’s pretty big. I’ve been flown around different cities and countries to share my story at conferences. I’ll admit, I’m always striving for that next thing, always wanting to do more to help others. So I try to remember to take a step back and be proud of what I’ve already done and the positive impact I’ve had on other people’s lives. Speaking gigs, where I talk in front of thousands of people, are really amazing (I used to get scared speaking in front of my classmates!) but I’ve realized it’s those smaller moments of connection - where I meet with people from the audience - that feel most impactful.
Over the years, I’ve made countless connections with people that reached out to me from seeing my content. The Associated Press included me in a documentary with various people experiencing lung infections (some CF related, some not). They wanted to learn about phage treatment. I connected with a lot of people during that time and was so happy to provide that kind of support and guidance. I was also part of a documentary called Silent Pandemic, where they chronicled journeys of people living with antimicrobial resistance (AMR). As mentioned, the bacteria in my lungs form resistance to the antibiotics. It’s been shared globally and has had a huge impact because of the sheer volume of people that have seen it. Hopefully it will bring more awareness to AMR and at some point down the line, inspire new research.
Another memorable connection I made was at the National Cystic Fibrosis Conference. I was walking around the exhibit hall where they had different research posters. I found a researcher who was working on phage therapy. I put two and two together and realized that the phage he was researching was the one I had taken. So I said to him, “I received a phage! The names of these look familiar to me. I’m a patient.” He was blown away. He said, “Oh my gosh, I have worked with your bacteria samples. I tested them!” He’s been doing this work for years and years in the lab, but never had the chance to actually meet a patient he had sampled. It was a really impactful moment for us both.

I’m making up for those early years
When I reflect back on all those years where I didn’t want to talk about my CF, I think it was because I was afraid of people’s judgment. But the less I care about what others think, the more I realize that most people are genuinely just curious. If given the opportunity to get to know you, they really do listen and care. That’s changed my perspective and made me more open to sharing with other people. I think there’s always an element of fear whenever you share something about yourself, but the more I’ve done it, the easier it’s become.
My advocacy work has always kept me really occupied, especially now that my health is more stabilized. I don’t like to wallow or dwell on things; I’ve found that there’s no use in that. If I am going to make the most of this life, I’m going to focus on the things I can control and try to let go of the rest. It’s really helped me become more social. I now have large networks both professionally and socially with friends. I’ve traveled a lot. I’ve done a lot of things. I guess in a way I’m making up for those early years. That’s maybe the catalyst for how I show up in the world now. I also just love new experiences and adventures. I like excitement! I really care about living my life to the fullest because I don’t know what things look like for me long-term. I work really hard to take care of my health as best as I can, and I stay very tuned in to the care I receive.
Writing is incredibly meaningful and cathartic for me. But I’ll admit, I’m not always consistent with it! There have been times - especially in 2018 - when my health had to be in the forefront of my mind. Every hour of every day I was struggling to live because of infections. So I didn’t write as much. But even now, despite the fact that my health has taken more of a backseat, my writing has still gotten away from me. I haven’t done as much introspection and sharing. Sometimes I’ll say to myself, “Have you turned cold? Why are you not inspired to write or share your feelings?” But I think it’s because I’m more concerned with other day-to-day things like working with new companies, being on new advisory boards, traveling for conferences, and meeting people in the rare disease community. It’s become my passion.
Cystic fibrosis has been my greatest curse and my greatest blessing. I’ve dealt with a lot of very difficult health obstacles and challenges in various ways. But I wouldn’t have gained the resilience and perspective I now have without it. I’d be more caught up in the insignificant things in life that really don’t matter, and might not be striving to live my life to the fullest as I am now. My experiences have taught me who I am and how to live my life. I wouldn’t change it.”
.avif)
To learn more about Ella’s journey and advocacy, visit her website here: https://www.ellabalasa.com/
“Growing up, I hated being different. I was afraid of people knowing I was sick. I had some friends, but I was insecure, which made me very reserved, uneasy, and afraid to be myself. I struggled to make genuine friendships. My parents were very supportive. They were always there for me and when I was hospitalized, they would take turns staying with me so that I was never alone. They were also very protective. I think I understand why - they were just looking out for me - but it sheltered me. Today, I’m pretty outgoing, friendly, personable, and social. It took time, though!
Cystic Fibrosis is an invisible disease. Because of that, people have a hard time understanding the gravity of it. No one really knows how sick you are because they can’t “see” it. When you look fine on the outside, people assume you are fine. I mean, sure, people can sometimes see when I'm out of breath, and if you lived with me you’d see that I’m coughing all the time and using oxygen. But other than that, it’s hard for people to grasp. It doesn’t bother me as much anymore, but there was a time when it was really frustrating. I felt so misunderstood. I want to help people realize just how difficult it really is.
I was diagnosed when I was 18 months old
I was very sickly as an infant and always at the pediatrician’s office. They didn’t know what was wrong with me for a while. When my parents learned I had a genetic lung condition called Cystic Fibrosis (CF), they were terrified. They had never heard of it before. It’s a life-shortening disease, because it ultimately results in lung failure. The doctors told them I’d live into my late teens or early twenties (I am 32 years old now).
CF causes a buildup of mucus in the lungs. Three to four times a day I have to use a nebulizer with aerosolized medication to clear my airways. The treatment makes the mucus thinner so that I can cough it out, because that’s the only way to expel it. But the mucus attracts bacterial infections, which require intravenous antibiotics to treat them. I've had countless lung infections over the course of my life, so I'm very familiar with these treatments. I’d be in the hospital for three weeks at a time, multiple times a year. As I’ve gotten older, the infections have become more and more difficult to treat, because the frequent antibiotic use has led to antibiotic resistance. So there are now less antibiotics that work effectively against the bacteria. And the ones that do work take a long time to work. Most people are at 100% lung function. I’ve had less than 40% lung function for over 10 years, which is pretty low. Currently, it’s at around 28%. It’s been a slow decline.
CF is also a multi-organ-affecting disease. For most people with CF, the pancreas is also affected, which harms the production of digestive enzymes that break down food when you eat it. My pancreas doesn't produce these enzymes at all, so I have to take artificial enzyme pills when I eat. They're not as effective as our own bodies’ enzymes, so a lot of people with CF are underweight and have stomach problems. There can also be liver issues, sinus/upper respiratory issues, and CF related diabetes for some people. But not everyone is affected the same way.
I learned to accept my life exactly as it was
I went to catholic school for elementary school. It was a very small community. All the teachers knew me, so that gave me some comfort. I went to a public high school, because I wanted that experience too. But it was harsher than I expected, so I really never came out of my shell. I didn’t have many friends.
For college, I stayed local instead of going away. Part of that was my parents’ influence; they wanted to keep me close to ensure I was properly cared for by doctors. But if I’m honest, I was also scared to be on my own. So I commuted to and from school the first two years. It felt like life was “same old, same old.” I was just so unfulfilled. Eventually a shift started to happen within me, where I realized something had to change. During the spring of my sophomore year, I was really sick and in the hospital. My lungs were in bad shape and the doctors said I would likely need a transplant. It was the worst possible news. A lung transplant is a huge surgery. There’s no guarantee that it will work or that you will survive. So I had this intense moment where I knew so clearly that I didn’t want my life to end without living it first. It changed everything for me. I said to myself, “Oh my God, I might die and I haven’t lived the life that I want. Something has to change. My life has to change and only I can do that.”
Fortunately, I didn’t end up needing a transplant. But from that point on, I really started to push outside my comfort zone, whether that was meeting new people or having new experiences. I joined a sorority and started to feel more comfortable in accepting my CF diagnosis. I learned to accept my life exactly as it was and decided I was going to make the very most of it.
I err on the side of risk
In 2018, I got sick with a pretty bad infection. My lung function was at 18%. So I was taking antibiotics and on oxygen 24/7 for a couple of weeks. During that time, a company reached out to me, asking if I’d write an article for them about what it’s like to live with CF (I had started blogging prior to that, as a way to share my story and my introspective journey). They were hoping my story could accompany a short documentary they were working on. They sent me the documentary to watch, and it was all about a CF patient who was being treated at Yale with an experimental treatment called phage therapy. I had heard about phage, but didn’t know much about it. And I definitely didn’t know that someone with CF could be treated with it. Since I have a biology background, I of course started researching it and thought to myself, “I’m really, really sick and antibiotics aren’t working. They’re not a sustainable treatment option. I want to try this.”
I reached out to the researchers at Yale that day. I told them I saw the documentary and asked if they’d treat me. They got back to me really quickly. We had a long conversation about the pros and cons, and I found out there was actually minimal risk involved. They asked me to send a sample of the mucus from my lungs so they could test the bacteria, to determine the right treatment course. So I did that. I also had an appointment with my CF doctor and told him I wanted to try it. He said, “There’s no research on this. It’s not FDA approved, and it’s not even in clinical trials yet.” He was skeptical, but ultimately the decision was mine to make.
I’d say I err on the side of taking risks - maybe more so than the average person. But I was so sick and knew if I didn’t try something different, I might not live. I was certainly afraid that the treatment could make me worse and even kill me. But it was a dire situation. I was desperate. So I made the decision for myself to move forward with the phage treatment. I’m lucky that my family has always been so supportive of me. They respect and value my knowledge about my own care and trust my decision-making process. I traveled up to Yale for the treatment. My mom drove me while I laid in the back seat. The coughing and fatigue were just unbearable. It’s really scary thinking about navigating this alone. I don’t take my support system for granted!
I don’t really believe in miracles, but the serendipity of it all was truly amazing
I was treated with phage therapy for a week at Yale, but didn’t feel much different after. I came back home to Richmond and saw my CF doctor a few days later. He said, “Well, you tried it. But nothing’s changed. You’re very sick, and we should move forward with you getting a lung transplant.” There’s nowhere to get a transplant in Richmond, so I went to Duke University hospital in North Carolina. I was admitted to the hospital there getting IV antibiotics, and for some testing and prep for the transplant. But a couple days later, I started clearing out my infection. I had taken these antibiotics before but never had results like this. So I called the researchers at Yale, and we realized that the phage therapy had changed my bacterial sensitivities. The synergy of the phage and the antibiotic working together helped to kill the bacteria and subdue the acute infection. The serendipity of it all was truly amazing. If that company hadn’t reached out about writing a blog article, I wouldn’t have known about the phage treatment as an option, and likely could have been transplanted or a worse outcome that I don’t want to think about.
After I received that experimental treatment and realized it helped, my first thought was that I wanted to make other people with CF aware of it. I’ve become a big advocate for phage therapy and the development of novel therapeutics against antimicrobial resistant infections, because it’s the greatest threat to my life and anyone else living with CF. I also wanted to share my story in the hopes of inspiring others to pursue all of their options, whether that be trying an experimental treatment option, pursuing a different care option they hadn’t yet considered, or fighting their insurance company to approve a drug that could help them. I want people to take ownership of their care and push the boundaries, to see what they can achieve and if they can improve their health outcomes. I wrote an article about this and tried to get it published all over. Eventually HuffPost picked it up!
If I let my emotions take control of my mind, I’ll fall apart
Returning to what happened after the phage treatment and infection: because my body was very weak and I still had very low lung function, I decided to continue the evaluation process for transplant. But as luck would have it, a few months later as I was to be listed on the waitlist for getting new lungs, a drug was approved to treat the underlying cause of CF. So I started that drug and it stabilized me, reducing the mucus and bacterial burden in my lungs. I didn’t need the transplant as imminently anymore. The treatment doesn’t cure CF, but it slows its progression. I’ve had less infections since then and haven’t needed IV antibiotics in these last four years. It’s amazing. I still use inhaled and oral antibiotics every few months to treat lingering symptoms, I still do breathing treatments a few times a day, and I still use oxygen when I exercise and sleep. I certainly have pushed my body and do as much as I can within the limits that I have. Sometimes when I’m winded and there's a flight of stairs, I think to myself, “Ok, let’s do this.” Sometimes I can, sometimes I can’t. But my mind always wants to try.
Eventually I know my body is going to say to me, “That’s it, we have nothing left to give.” But until then, I keep pushing. It might be a coping mechanism, because if I let my emotions take control of my mind, I’ll fall apart. So I keep it moving. I just have this grit to survive. When I’ve had periods of doom - like in 2019 when I was out of breath just putting my hands over my head to wash my hair in the shower - I relied on grit. I’d focus on making it just one more hour, one more day.

I am surprised by how far I’ve made it
And I don’t mean the length of the time that I’ve lived, but rather what I’ve accomplished. I am not someone who brags about themselves or the amazing things they’ve done in their life. That’s not me. But if I really think about it from a purely factual, objective way - in terms of the impact I’ve had on the rare disease community - it’s pretty big. I’ve been flown around different cities and countries to share my story at conferences. I’ll admit, I’m always striving for that next thing, always wanting to do more to help others. So I try to remember to take a step back and be proud of what I’ve already done and the positive impact I’ve had on other people’s lives. Speaking gigs, where I talk in front of thousands of people, are really amazing (I used to get scared speaking in front of my classmates!) but I’ve realized it’s those smaller moments of connection - where I meet with people from the audience - that feel most impactful.
Over the years, I’ve made countless connections with people that reached out to me from seeing my content. The Associated Press included me in a documentary with various people experiencing lung infections (some CF related, some not). They wanted to learn about phage treatment. I connected with a lot of people during that time and was so happy to provide that kind of support and guidance. I was also part of a documentary called Silent Pandemic, where they chronicled journeys of people living with antimicrobial resistance (AMR). As mentioned, the bacteria in my lungs form resistance to the antibiotics. It’s been shared globally and has had a huge impact because of the sheer volume of people that have seen it. Hopefully it will bring more awareness to AMR and at some point down the line, inspire new research.
Another memorable connection I made was at the National Cystic Fibrosis Conference. I was walking around the exhibit hall where they had different research posters. I found a researcher who was working on phage therapy. I put two and two together and realized that the phage he was researching was the one I had taken. So I said to him, “I received a phage! The names of these look familiar to me. I’m a patient.” He was blown away. He said, “Oh my gosh, I have worked with your bacteria samples. I tested them!” He’s been doing this work for years and years in the lab, but never had the chance to actually meet a patient he had sampled. It was a really impactful moment for us both.

I’m making up for those early years
When I reflect back on all those years where I didn’t want to talk about my CF, I think it was because I was afraid of people’s judgment. But the less I care about what others think, the more I realize that most people are genuinely just curious. If given the opportunity to get to know you, they really do listen and care. That’s changed my perspective and made me more open to sharing with other people. I think there’s always an element of fear whenever you share something about yourself, but the more I’ve done it, the easier it’s become.
My advocacy work has always kept me really occupied, especially now that my health is more stabilized. I don’t like to wallow or dwell on things; I’ve found that there’s no use in that. If I am going to make the most of this life, I’m going to focus on the things I can control and try to let go of the rest. It’s really helped me become more social. I now have large networks both professionally and socially with friends. I’ve traveled a lot. I’ve done a lot of things. I guess in a way I’m making up for those early years. That’s maybe the catalyst for how I show up in the world now. I also just love new experiences and adventures. I like excitement! I really care about living my life to the fullest because I don’t know what things look like for me long-term. I work really hard to take care of my health as best as I can, and I stay very tuned in to the care I receive.
Writing is incredibly meaningful and cathartic for me. But I’ll admit, I’m not always consistent with it! There have been times - especially in 2018 - when my health had to be in the forefront of my mind. Every hour of every day I was struggling to live because of infections. So I didn’t write as much. But even now, despite the fact that my health has taken more of a backseat, my writing has still gotten away from me. I haven’t done as much introspection and sharing. Sometimes I’ll say to myself, “Have you turned cold? Why are you not inspired to write or share your feelings?” But I think it’s because I’m more concerned with other day-to-day things like working with new companies, being on new advisory boards, traveling for conferences, and meeting people in the rare disease community. It’s become my passion.
Cystic fibrosis has been my greatest curse and my greatest blessing. I’ve dealt with a lot of very difficult health obstacles and challenges in various ways. But I wouldn’t have gained the resilience and perspective I now have without it. I’d be more caught up in the insignificant things in life that really don’t matter, and might not be striving to live my life to the fullest as I am now. My experiences have taught me who I am and how to live my life. I wouldn’t change it.”
.avif)
To learn more about Ella’s journey and advocacy, visit her website here: https://www.ellabalasa.com/
“Growing up, I hated being different. I was afraid of people knowing I was sick. I had some friends, but I was insecure, which made me very reserved, uneasy, and afraid to be myself. I struggled to make genuine friendships. My parents were very supportive. They were always there for me and when I was hospitalized, they would take turns staying with me so that I was never alone. They were also very protective. I think I understand why - they were just looking out for me - but it sheltered me. Today, I’m pretty outgoing, friendly, personable, and social. It took time, though!
Cystic Fibrosis is an invisible disease. Because of that, people have a hard time understanding the gravity of it. No one really knows how sick you are because they can’t “see” it. When you look fine on the outside, people assume you are fine. I mean, sure, people can sometimes see when I'm out of breath, and if you lived with me you’d see that I’m coughing all the time and using oxygen. But other than that, it’s hard for people to grasp. It doesn’t bother me as much anymore, but there was a time when it was really frustrating. I felt so misunderstood. I want to help people realize just how difficult it really is.
I was diagnosed when I was 18 months old
I was very sickly as an infant and always at the pediatrician’s office. They didn’t know what was wrong with me for a while. When my parents learned I had a genetic lung condition called Cystic Fibrosis (CF), they were terrified. They had never heard of it before. It’s a life-shortening disease, because it ultimately results in lung failure. The doctors told them I’d live into my late teens or early twenties (I am 32 years old now).
CF causes a buildup of mucus in the lungs. Three to four times a day I have to use a nebulizer with aerosolized medication to clear my airways. The treatment makes the mucus thinner so that I can cough it out, because that’s the only way to expel it. But the mucus attracts bacterial infections, which require intravenous antibiotics to treat them. I've had countless lung infections over the course of my life, so I'm very familiar with these treatments. I’d be in the hospital for three weeks at a time, multiple times a year. As I’ve gotten older, the infections have become more and more difficult to treat, because the frequent antibiotic use has led to antibiotic resistance. So there are now less antibiotics that work effectively against the bacteria. And the ones that do work take a long time to work. Most people are at 100% lung function. I’ve had less than 40% lung function for over 10 years, which is pretty low. Currently, it’s at around 28%. It’s been a slow decline.
CF is also a multi-organ-affecting disease. For most people with CF, the pancreas is also affected, which harms the production of digestive enzymes that break down food when you eat it. My pancreas doesn't produce these enzymes at all, so I have to take artificial enzyme pills when I eat. They're not as effective as our own bodies’ enzymes, so a lot of people with CF are underweight and have stomach problems. There can also be liver issues, sinus/upper respiratory issues, and CF related diabetes for some people. But not everyone is affected the same way.
I learned to accept my life exactly as it was
I went to catholic school for elementary school. It was a very small community. All the teachers knew me, so that gave me some comfort. I went to a public high school, because I wanted that experience too. But it was harsher than I expected, so I really never came out of my shell. I didn’t have many friends.
For college, I stayed local instead of going away. Part of that was my parents’ influence; they wanted to keep me close to ensure I was properly cared for by doctors. But if I’m honest, I was also scared to be on my own. So I commuted to and from school the first two years. It felt like life was “same old, same old.” I was just so unfulfilled. Eventually a shift started to happen within me, where I realized something had to change. During the spring of my sophomore year, I was really sick and in the hospital. My lungs were in bad shape and the doctors said I would likely need a transplant. It was the worst possible news. A lung transplant is a huge surgery. There’s no guarantee that it will work or that you will survive. So I had this intense moment where I knew so clearly that I didn’t want my life to end without living it first. It changed everything for me. I said to myself, “Oh my God, I might die and I haven’t lived the life that I want. Something has to change. My life has to change and only I can do that.”
Fortunately, I didn’t end up needing a transplant. But from that point on, I really started to push outside my comfort zone, whether that was meeting new people or having new experiences. I joined a sorority and started to feel more comfortable in accepting my CF diagnosis. I learned to accept my life exactly as it was and decided I was going to make the very most of it.
I err on the side of risk
In 2018, I got sick with a pretty bad infection. My lung function was at 18%. So I was taking antibiotics and on oxygen 24/7 for a couple of weeks. During that time, a company reached out to me, asking if I’d write an article for them about what it’s like to live with CF (I had started blogging prior to that, as a way to share my story and my introspective journey). They were hoping my story could accompany a short documentary they were working on. They sent me the documentary to watch, and it was all about a CF patient who was being treated at Yale with an experimental treatment called phage therapy. I had heard about phage, but didn’t know much about it. And I definitely didn’t know that someone with CF could be treated with it. Since I have a biology background, I of course started researching it and thought to myself, “I’m really, really sick and antibiotics aren’t working. They’re not a sustainable treatment option. I want to try this.”
I reached out to the researchers at Yale that day. I told them I saw the documentary and asked if they’d treat me. They got back to me really quickly. We had a long conversation about the pros and cons, and I found out there was actually minimal risk involved. They asked me to send a sample of the mucus from my lungs so they could test the bacteria, to determine the right treatment course. So I did that. I also had an appointment with my CF doctor and told him I wanted to try it. He said, “There’s no research on this. It’s not FDA approved, and it’s not even in clinical trials yet.” He was skeptical, but ultimately the decision was mine to make.
I’d say I err on the side of taking risks - maybe more so than the average person. But I was so sick and knew if I didn’t try something different, I might not live. I was certainly afraid that the treatment could make me worse and even kill me. But it was a dire situation. I was desperate. So I made the decision for myself to move forward with the phage treatment. I’m lucky that my family has always been so supportive of me. They respect and value my knowledge about my own care and trust my decision-making process. I traveled up to Yale for the treatment. My mom drove me while I laid in the back seat. The coughing and fatigue were just unbearable. It’s really scary thinking about navigating this alone. I don’t take my support system for granted!
I don’t really believe in miracles, but the serendipity of it all was truly amazing
I was treated with phage therapy for a week at Yale, but didn’t feel much different after. I came back home to Richmond and saw my CF doctor a few days later. He said, “Well, you tried it. But nothing’s changed. You’re very sick, and we should move forward with you getting a lung transplant.” There’s nowhere to get a transplant in Richmond, so I went to Duke University hospital in North Carolina. I was admitted to the hospital there getting IV antibiotics, and for some testing and prep for the transplant. But a couple days later, I started clearing out my infection. I had taken these antibiotics before but never had results like this. So I called the researchers at Yale, and we realized that the phage therapy had changed my bacterial sensitivities. The synergy of the phage and the antibiotic working together helped to kill the bacteria and subdue the acute infection. The serendipity of it all was truly amazing. If that company hadn’t reached out about writing a blog article, I wouldn’t have known about the phage treatment as an option, and likely could have been transplanted or a worse outcome that I don’t want to think about.
After I received that experimental treatment and realized it helped, my first thought was that I wanted to make other people with CF aware of it. I’ve become a big advocate for phage therapy and the development of novel therapeutics against antimicrobial resistant infections, because it’s the greatest threat to my life and anyone else living with CF. I also wanted to share my story in the hopes of inspiring others to pursue all of their options, whether that be trying an experimental treatment option, pursuing a different care option they hadn’t yet considered, or fighting their insurance company to approve a drug that could help them. I want people to take ownership of their care and push the boundaries, to see what they can achieve and if they can improve their health outcomes. I wrote an article about this and tried to get it published all over. Eventually HuffPost picked it up!
If I let my emotions take control of my mind, I’ll fall apart
Returning to what happened after the phage treatment and infection: because my body was very weak and I still had very low lung function, I decided to continue the evaluation process for transplant. But as luck would have it, a few months later as I was to be listed on the waitlist for getting new lungs, a drug was approved to treat the underlying cause of CF. So I started that drug and it stabilized me, reducing the mucus and bacterial burden in my lungs. I didn’t need the transplant as imminently anymore. The treatment doesn’t cure CF, but it slows its progression. I’ve had less infections since then and haven’t needed IV antibiotics in these last four years. It’s amazing. I still use inhaled and oral antibiotics every few months to treat lingering symptoms, I still do breathing treatments a few times a day, and I still use oxygen when I exercise and sleep. I certainly have pushed my body and do as much as I can within the limits that I have. Sometimes when I’m winded and there's a flight of stairs, I think to myself, “Ok, let’s do this.” Sometimes I can, sometimes I can’t. But my mind always wants to try.
Eventually I know my body is going to say to me, “That’s it, we have nothing left to give.” But until then, I keep pushing. It might be a coping mechanism, because if I let my emotions take control of my mind, I’ll fall apart. So I keep it moving. I just have this grit to survive. When I’ve had periods of doom - like in 2019 when I was out of breath just putting my hands over my head to wash my hair in the shower - I relied on grit. I’d focus on making it just one more hour, one more day.

I am surprised by how far I’ve made it
And I don’t mean the length of the time that I’ve lived, but rather what I’ve accomplished. I am not someone who brags about themselves or the amazing things they’ve done in their life. That’s not me. But if I really think about it from a purely factual, objective way - in terms of the impact I’ve had on the rare disease community - it’s pretty big. I’ve been flown around different cities and countries to share my story at conferences. I’ll admit, I’m always striving for that next thing, always wanting to do more to help others. So I try to remember to take a step back and be proud of what I’ve already done and the positive impact I’ve had on other people’s lives. Speaking gigs, where I talk in front of thousands of people, are really amazing (I used to get scared speaking in front of my classmates!) but I’ve realized it’s those smaller moments of connection - where I meet with people from the audience - that feel most impactful.
Over the years, I’ve made countless connections with people that reached out to me from seeing my content. The Associated Press included me in a documentary with various people experiencing lung infections (some CF related, some not). They wanted to learn about phage treatment. I connected with a lot of people during that time and was so happy to provide that kind of support and guidance. I was also part of a documentary called Silent Pandemic, where they chronicled journeys of people living with antimicrobial resistance (AMR). As mentioned, the bacteria in my lungs form resistance to the antibiotics. It’s been shared globally and has had a huge impact because of the sheer volume of people that have seen it. Hopefully it will bring more awareness to AMR and at some point down the line, inspire new research.
Another memorable connection I made was at the National Cystic Fibrosis Conference. I was walking around the exhibit hall where they had different research posters. I found a researcher who was working on phage therapy. I put two and two together and realized that the phage he was researching was the one I had taken. So I said to him, “I received a phage! The names of these look familiar to me. I’m a patient.” He was blown away. He said, “Oh my gosh, I have worked with your bacteria samples. I tested them!” He’s been doing this work for years and years in the lab, but never had the chance to actually meet a patient he had sampled. It was a really impactful moment for us both.

I’m making up for those early years
When I reflect back on all those years where I didn’t want to talk about my CF, I think it was because I was afraid of people’s judgment. But the less I care about what others think, the more I realize that most people are genuinely just curious. If given the opportunity to get to know you, they really do listen and care. That’s changed my perspective and made me more open to sharing with other people. I think there’s always an element of fear whenever you share something about yourself, but the more I’ve done it, the easier it’s become.
My advocacy work has always kept me really occupied, especially now that my health is more stabilized. I don’t like to wallow or dwell on things; I’ve found that there’s no use in that. If I am going to make the most of this life, I’m going to focus on the things I can control and try to let go of the rest. It’s really helped me become more social. I now have large networks both professionally and socially with friends. I’ve traveled a lot. I’ve done a lot of things. I guess in a way I’m making up for those early years. That’s maybe the catalyst for how I show up in the world now. I also just love new experiences and adventures. I like excitement! I really care about living my life to the fullest because I don’t know what things look like for me long-term. I work really hard to take care of my health as best as I can, and I stay very tuned in to the care I receive.
Writing is incredibly meaningful and cathartic for me. But I’ll admit, I’m not always consistent with it! There have been times - especially in 2018 - when my health had to be in the forefront of my mind. Every hour of every day I was struggling to live because of infections. So I didn’t write as much. But even now, despite the fact that my health has taken more of a backseat, my writing has still gotten away from me. I haven’t done as much introspection and sharing. Sometimes I’ll say to myself, “Have you turned cold? Why are you not inspired to write or share your feelings?” But I think it’s because I’m more concerned with other day-to-day things like working with new companies, being on new advisory boards, traveling for conferences, and meeting people in the rare disease community. It’s become my passion.
Cystic fibrosis has been my greatest curse and my greatest blessing. I’ve dealt with a lot of very difficult health obstacles and challenges in various ways. But I wouldn’t have gained the resilience and perspective I now have without it. I’d be more caught up in the insignificant things in life that really don’t matter, and might not be striving to live my life to the fullest as I am now. My experiences have taught me who I am and how to live my life. I wouldn’t change it.”
.avif)
To learn more about Ella’s journey and advocacy, visit her website here: https://www.ellabalasa.com/
Be a voice for the patient to the best of your ability, and don’t be discouraged or afraid to relay both your needs and the patients’ needs when it comes to advocating in healthcare settings. You have vast knowledge of the patients’ health, what works, what doesn’t, and in circumstances when the patient cannot be their own best advocate, don’t be afraid to step up.
Representation Matters
Increasing diversity in clinical trials builds trust, promotes health equity, and leads to more effective treatments and better outcomes (NEJM). But there is much work to be done - and barriers to break - to improve awareness and access for all people.
Do you know someone who is a member of a marginalized community who has participated in a clinical trial? If so, we’d love to meet them and share their story. We hope to represent the many faces of clinical trials through this project, and inspire others by shining a light on their experience.
They can contact us here.


