“It was cancer the entire time. But no one believed me.”

I’m Laurie, and I’m 64 years old. I grew up in the Northeast, went to a small liberal arts college in upstate New York, and worked at a bank in Boston after graduation. In 1984, I accepted a job offer in Los Angeles. I packed up, moved west, and worked for a small startup software company. The transition was hard; LA can be a very lonely city if you don't have an established network. But I threw myself into my work. For a few years, I was bicoastal: two weeks in Manhattan and two weeks in LA. I had an apartment in both cities.
Before cancer, I was enjoying life, although my priority was always my career. I married late, had my son at 40, and had a successful, longtime career in financial services. I worked for the same company for nearly 25 years and eventually became president of the firm. I had a great run. But my job back then was to help other people make money. I was constantly working on the next thing: the next business product, the next market, the next board meeting. I was traveling internationally regularly. That said, after a 12-year, life-threatening cancer journey, I never went back to financial services. It held no appeal anymore. I had a rude, sudden awakening that I needed to stay focused on my health and help other cancer patients on their journeys.
A couple years after my diagnosis, it was clear the cancer wasn’t retreating and I needed to leave my work. When I stopped working, my son was going into third grade. I approached his teacher, shared my cancer journey, and offered to help in the classroom every morning, doing tasks like sharpening pencils and checking homework. It was weird (and I like to think nice) for my son to see me present every day, a stark contrast to my previous absence. But the blinders came off and I realized my priorities had been seriously misplaced.

I was dismissed by doctors for a good two years
It all started when I was 43 and experiencing frequent sinus infections. New symptoms kept appearing, including a very dry eye. I had been a contact lens wearer for 30 years and suddenly I couldn’t wear them anymore. I felt exhausted and had a gut feeling that something was very wrong. I went to a few doctors and they blamed hormones and allergies. I had an enlarged lymph node in my neck, and for that, they blamed sinus infections. As to the lump I felt in my abdomen, they said it was likely a hernia. Part of me really wanted to believe they were right and that nothing was wrong. But I just knew the doctors were wrong. I eventually took my husband to some of my appointments; he was shocked at the way the doctors treated me.
In the Spring of 2006, I went to “the best” ear, nose, and throat doctor in Los Angeles (I roll my eyes when I say this now as I know there is no such thing). I had done a Google search of my symptoms (as one does, right?) and was worried that my sinus infections were related to lymphoma. My husband joined me for the consult, as I felt his being there would be helpful. When I shared my symptoms with the doctor and said I was worried I might have lymphoma, he looked at my husband and rolled his eyes as if I were some stupid blonde. He then looked at me and said, “How did you even come up with that idea?” I replied, “The Internet.” He went, “Ah, Dr. Google. Well, I went to Med school for 12 years and did a residency plus a fellowship.” He looked at my husband and rolled his eyes again. It was infuriating, just unbelievable. He then said, “You don’t have lymphoma. If you let me treat you for your allergies, you’re going to be fine.” I replied, “Doctor, that’s all fine and good, but I got tested for allergies and I don’t have any allergies. I’ve never had allergies.”
I shared with him that I also was really fatigued all the time. Once again, he rolled his eyes and said, “Well, what do you think that could be from? You're running a company, traveling to London and New York regularly, all while running a household with a little kid at home. I'm tired just listening to you. Your blood work is all normal. You're fine. You just have allergies."
I wanted to believe him, but in my heart, I knew.
I wanted to get another opinion, so I called an old friend in LA and asked if she knew a diagnostician. She recommended someone nearby and a couple weeks later, I saw him. He agreed that it could be a hernia, sinus issues, hormonal changes, or dry eyes. “But we don’t make guesses about this stuff. That’s why we have CT machines,” he said. Out of the many doctors I had seen, he was the first to order a CT of my abdomen to confirm it was a hernia. Two days after the CT, I received a call and was told I needed to come in that same day, which happened to be Good Friday in 2006. My son was in kindergarten at the time of my diagnosis. I learned I had either a mesenchymal tumor that would likely be fatal within 30 days, or some kind of lymphoma. He made an appointment for me with an oncologist for the following Monday at an oncology practice. I said, “I can’t go on Monday. I have to fly to New York and Chicago because I’m having my annual client conferences. We have 300 of our clients coming and I’m giving the keynote speech.” He looked at me like I was a bit crazy but told me fine, and that as soon as I was back, I’d need to get on it right away.
We continued talking and suddenly, it all hit me. I said, “I guess I’m not going to New York and Chicago, am I?” He replied, “I certainly hope not.”
I wanted to be anybody but me
I had the PET-CT that Monday. I remember being in the car as my husband drove me to the appointment. I saw a sanitation worker emptying a trash can and wished I could switch places with him. I wanted to be anybody but me. My body had completely let me down. I thought, “How could this happen to me?” I had never smoked or engaged in cancer-causing activities. Where had I gone wrong? I was trying so hard to point fingers at myself. But I quickly learned it can all just be random. And it’s not your fault.
The scans confirmed I had stage 4 follicular Non Hodgkin's lymphoma. They said given the size of the tumor, I had likely had it for at least five years, meaning I could have had it when I was pregnant with my son. So that “hernia” in my abdomen I had told my doctor about? It was, in fact, a giant metastasized tumor the size of a grapefruit. And the dry eye? That was because I had a tumor blocking my tear duct.
It was cancer the entire time. But no one believed me.
One of the first things I did was write a letter to the ENT doctor who ignored me. “I was the blonde lady who came in concerned she had lymphoma. You were completely dismissive and insulting. You rolled your eyes at my husband when I asked if I had lymphoma. I just learned that in fact I do have lymphoma and it’s stage 4. I hope the next time a patient comes in, you won’t roll your eyes at them and dismiss their concerns. Listen to them. Listen to your patient.”
It felt good writing that letter. I was never going to take action - I wasn’t going to file a suit - but maybe I raised his awareness a bit.
I remember not knowing whether I should even tell my son I was sick. But my oncologist said, “You're going to lose your hair from the chemo. If you don’t tell him, he’ll go to school, tell his friends his mom lost her hair, and they’ll say something like ‘Oh, that happened to my grandma too. She died from cancer.’ I realized I needed to get in front of it, so we told my son right away. He said, “But Mommy, girls aren’t bald!” But then he said, "Oh, wait, you're gonna be bald, Mommy…COOL”!" The way he said it…it was as if it was the coolest thing in the world. It was really sweet. But it was also really hard. That same night my husband and I told him about my illness, my son called me into his room after lights out. He said, "Mommy, will you come in here because I'm really worried." I said, "What's the matter?" And he said, "You're going to be bald. Is everybody going to make fun of you?" I said, "Oh, no, I will wear a wig, scarf and hats. Nobody's going to know. Don't worry, it will be fine. And when my hair starts to fall out, you can help me pull it out and we’ll donate it."
My son had a mom who had an incurable cancer and was in treatment for his entire childhood – his elementary, middle and high school years. He grew up fast. Even when he was young, he really stepped up. Of course he couldn't drive or go to the market and get groceries, but he could give me lots of love. He could climb into bed and hug me. He helped as much as he could around the house. I remember when he was in kindergarten, I told him that talking to someone about his feelings might help him feel better. But he insisted, "No, Mommy, I'm fine. I have to take care of you."
I had to start treatment right away because I was so sick and symptomatic
There was one approved treatment back in 2006, which was a chemo monoclonal antibody combination (the “big guns” as they called it). I started treatment in May of 2006 and took leave from my firm. On September 11, I had my sixth and final treatment. They scanned me and my disease was gone. I was told that since my disease responded so quickly, I would likely have a durable remission. I went back to work shortly after and resumed my crazy schedule and traveling. When I traveled, I wore a mask to keep other’s germs away from me, as the chemo had depleted my immune system – I think I was ahead of my time on the mask thing!
I received maintenance treatment every three months. In January the next year, they scanned me again and found out there was activity in my lungs. They said it could just be inflammation, but they recommended I see a pulmonologist and a lung surgeon. A lung biopsy is a really difficult thing to do, so we decided to just watch and wait, and gradually the disease was large enough that I had to find a new treatment.
When I was first diagnosed, I got four opinions. I’m lucky I live in LA because there are a lot of cancer hospitals. I made my rounds and they all agreed that if the chemo didn’t work, the next option would be an autologous stem cell transplant (SCT) with my own cells. So later on when my cancer came back after chemo, we had already harvested my stem cells as an insurance policy, should I ever need a transplant. But it’s a very difficult process and would require I get more brute force chemo. I also would be in the hospital for a month. I had done my own research on auto SCT and found that half of patients with my diagnosis relapsed in less than a year after a stem cell transplant. And, if you failed the type of chemo I had (which I did), the chances of durable remission after a stem cell transplant were very low.
I told the oncologist at the transplant center that I couldn’t do an SCT. I said, “I have a little kid at home. I can’t go to the hospital for a month. If it was a 90% chance of complete remission, then we’d make it work but at less than a 50% chance of durable remission, I just can’t do it. The odds for me just stink.”
He said to me, “Laurie, I’m going to find you a clinical trial.”
So I started my first clinical trial and while it didn’t shrink the tumor, it did stabilize it. I got a scan every three months and as long as you have a stable or smaller disease, you can continue on the trial. I felt so well-cared for in the trial as opposed to chemo, where I really felt like I was on my own. When I first enrolled, I was assigned a trial coordinator who efficiently organized all my appointments, biopsies, scans, and treatments. This made the process much more manageable. They provided continuous support and proactively checked in with me several times a week. From that point on, I was sold on clinical trials and convinced they would be part of my survival.
It felt like a death sentence
At my nine-month scan during that first clinical trial, my tumor had shrunk a little bit. My oncologist said, “Wow, this is a win. It’s shrinking. It’s working.” But at my one-year scan, it had grown. I was ousted from the trial. That said, in that one year period, new treatments had been approved, so I was given a new chemotherapy. This was my third line of treatment. I did chemo once a month for an entire year. My disease got smaller, but it was still present. We followed it up with a fourth treatment: radioimmunotherapy, which had just been approved. I spoke with patients who had been in the clinical trial for it; they were 10 years out and had complete remission. I thought to myself, “Treatment 4 will be different.” I thought for sure it was going to work.
A couple months after the radioimmunotherapy, I was reading and felt a tumor in the back of my neck. My cancer was back, and again, it was everywhere. It was as if the radioimmunotherapy had done nothing. My oncologist said the only option I had left was an allogeneic stem cell transplant, where you would get a new immune system from a donor. I saw multiple doctors and they all said the same thing: allo transplant. The patient gets more chemo to destroy the cancer, but it also destroys your immune system. Once the patient is in complete remission from the chemo, a donor’s stem cells are infused into you. It’s very risky. Many patients don’t make it out of the hospital. And the more heavily treated you are (like I was) the more likely you are to have problems.
The best donor is a sibling but neither of my two siblings were matches, so we looked into donor banks and discovered I had many matches - good news. But when you receive a donor’s stem cells and immune system, you can develop what's called graft versus host disease, where your new immune system starts to attack your existing organs. Doctors put patients on immune suppressors to minimize the risk, but this can lead to secondary cancer. The option of allo SCT terrified me.
It's an unbelievable story
I emailed a good friend of mine, letting her know I had relapsed again. She called me and said, “What are you doing right now?” I said, “I'm going to bed, I'm so depressed. I have to get up at three to pick up my son at school. But in the meantime, I'm going to bed.” She said, “No you're not. You’re going to turn your computer on, I'm going to come over, and we're going to find you another clinical trial. You are not going to do an allogeneic stem cell transplant.” She came over, we researched and found eight trials inside and outside the US - including one nearby at UCLA - and emailed the lead investigators for each. My friend left, I went back to bed, and an hour later my telephone rang. I looked at the caller ID and it said UCLA. I answered. “Laurie, this is the lead investigator at UCLA. I just read your email. I have a clinical trial that I think would work really well for you.” I immediately said, “But I'm so heavily treated and this will be my fifth line of therapy, why do you think it will work?” He said, “Because this drug is helping patients exactly like you who are heavily treated. Nothing else has worked for these patients, even those who’ve had transplants. But this is working for them. But I need you to come in today because it's a phase one trial, I have 19 people enrolled so far and I only have one spot left.”
I was supposed to attend and help set up a fundraiser that night for a non-profit blood cancer organization. I shared that with the oncologist, and coincidentally, he was also attending. We met that night at the event, and I reviewed and signed the trial paperwork. It's an unbelievable story - if my friend hadn’t insisted on coming over that day, none of this would have happened.
The trial was Phase 1 and it was testing a small molecule drug, a PI3 kinase inhibitor. The treatment was a pill I took in the morning and at night. Within days, my tumors were shrinking. I ended up being the “long tail” on that trial, which means I was the patient who was on the trial the longest. I was on the drug for almost six years – from spring 2011 until December 31, 2016. It had a GI side effect and it never put me in a complete remission, but it kept my disease stable and bought me loads of time for better options to come along.
It was a race against time for CAR-T Therapy
At the end of 2016, my cancer relapsed and I was removed from the Pi3 Kinase inhibitor trial. At that point, there was a new monoclonal antibody that had been approved, so I did that for 10 months and the tumor started to shrink and stabilize again. But as soon as I stopped that treatment, the cancer returned. I was in a race against time, hoping an immunotherapy called CAR-T cell therapy would become available in time to save my life. I had heard about CAR-T in 2012, but it wasn’t being tested for follicular NHL yet.
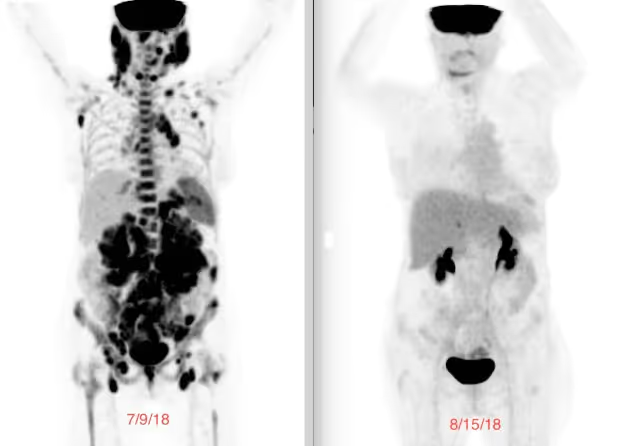
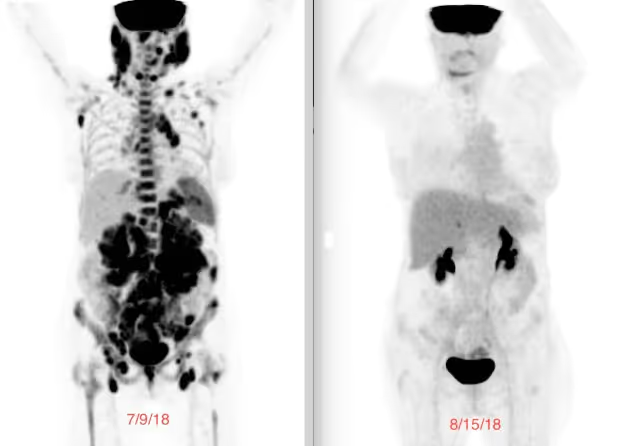
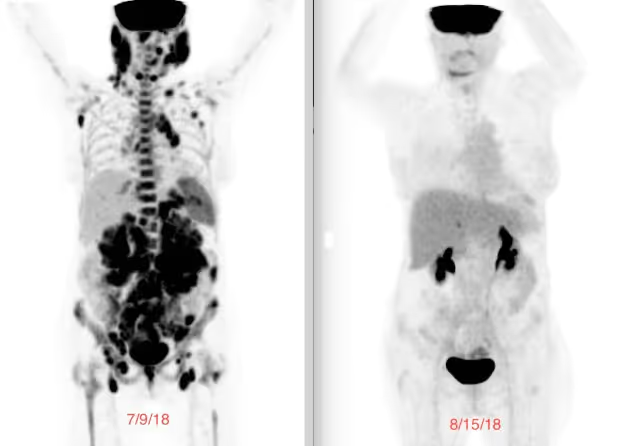
In Spring 2018, I got the call from my oncologist. “The CAR-T for fNHL trial is opening at UCLA. You will be the first of five patients to enroll.” I got the treatment July 16 and 30 days later, my cancer was completely gone and I was finally in a complete remission. The before and after scans were unbelievable…an estimated 8 pounds of tumor vanished as a result of CAR-T. I am now 6 years in complete remission post CAR-T. Follicular non-Hodgkin lymphoma has always been considered incurable, but my oncologist believes I'm cured. He said, “Laurie, you're done with lymphoma. Thanks to CAR-T, this cancer now has a cure.”
My little boy was my biggest motivator
I relapsed six times over the course of 12 years and was in continuous treatment all those years. People ask me, “Laurie, how did you do this? How did you keep going?” My motivator was my little boy. The thought of my husband having to tell my son that mommy died…it was just unfathomable. I said, I cannot let that happen. I have to fight. And if something doesn’t work, I have to find the next thing. I don't care what I have to do. I am not dying. My husband said, “What about me?” Of course I did not want to leave my husband either, but reminded him “You can get another wife, but our son cannot get another mom.”
Those 12 years felt like a roller coaster. Every time I would get optimistic, I’d get slammed down again. But I’d pick myself back up, brush myself off, and tell myself, “Find the next treatment, maybe it will work.” I vividly remember picking my son up from school when he was in the First Grade. I’d be waiting at the picnic bench when the class door would open and out he would run to me and jump into my arms. I’d say to myself, “I can’t miss these moments. I have to find the next treatment.”
I know I’m biased because I'm his mom, but my son was always caring and responsible. He worked multiple jobs starting at age 13. He delivered newspapers, had lemonade stands, and was a junior lifeguard and a skate guard at a local ice rink. Choosing a college was very tough for him: stay in LA or go away. We encouraged him to go away. It was hard for him after watching me fight my cancer, a cancer diagnosis impacts everyone in your life. So my son flew across the country to have his college experience. The summer I received CAR-T, he was certified as an EMT so could volunteer during his college years.
My husband and I have been together now for 30 years. During my cancer fight, I was strong and tried to keep my husband and my son out of everything as much as I could. My husband had a business to run, and I wanted him to focus on that while I dealt with the cancer. He used to say, "You're going to outlive me, you're so tuned in with all the medical details."

Swimming was my meditation
I found out early in my treatment that I needed to be active physically, mostly because I was a wreck emotionally. I was depressed and anxious. One day after a chemo treatment I said, "When I get home, I'm going to put on my tennis shoes, and I'm just going to walk to the end of the street." So I did that, and when I got back I thought, "That was really good." Not long after that, I started swimming. I had been taking my son to swim lessons at a local community college pool in Santa Monica. One day while he was in his lesson, I thought, "I'm going to go to the adult pool. I'm going to try to swim laps." I was still doing chemo and it was summer, so it was hot. Walking was hard because I’d get dizzy in the heat. So the pool seemed like a good alternative. I remember that first day I swam nearly 20 laps. It felt so great. It was slow - just like the walking - but it really helped me emotionally. I’ve never been able to meditate or do yoga. I’ve tried, but they’re just not for me. Lap swimming became my moving meditation.
I also went on an antidepressant. I felt like I needed to do everything I could to get my head working with my body. Day to day tasks at times were both physically and mentally challenging. I remember one time, a man walked up to me in the grocery store. I was wearing a scarf and he said “Oh, you must be doing chemo. How can you put that toxic stuff in your body, it will kill you! You just need a macrobiotic diet and you’ll be fine.” There was a woman in line, right in front of me, and she chimed in saying “Excuse me, what did you just say?” She reprimanded him. It turned out she was a survivor.
This experience has changed my life’s mission
Raising awareness of the game changing CAR-T immunotherapy and the benefit of clinical trials is my work now. People think of clinical trials from the scary stories of old. I was an early convert to clinical trials. Three of the seven treatments I had in my 12-year journey were clinical trials, and all three were provided at no cost to me. I learned quickly that clinical trials are often much smarter than standard of care therapies, they are more targeted and typically have fewer side effects. I’m a huge advocate for education around clinical trials.
There are access issues. Living in LA, I had access to multiple cancer centers for treatments and trials. During my 12-year journey, I was treated at four large cancer centers in Los Angeles. But many people are lucky if they have just one place in their state where they can access a trial. I’m trying to help change this. I work as a volunteer legislative advocate for the Leukemia & Lymphoma Society at both state and federal levels, to help make laws that require pharmaceutical companies to have more diversity in trials (racially, ethnically, geographically, and socioeconomically). I also work on advocating for patients and raising awareness of newer therapies, such as immunotherapies, which are more targeted. If you’re being treated at a community oncology center with an oncology generalist, they’re likely going to be doing what they’ve been doing for the past 30 years, which is chemo, transplant, and more chemo. They can’t possibly keep up to speed with all of the newer developments. I was an advocate for myself and I pushed and I pushed and I pushed. But not all patients can do that. Some aren’t equipped to be their own advocates due to language barriers, and some don’t have caregivers to help them. There are so many barriers, and because of that, we don’t have nearly enough diversity in clinical trials.
Cancer patients have such a tough road
I now spend about 20 hours a week as a cancer volunteer advocate for three different nonprofits. Helping others navigate their cancer journeys is something I am adept at. I’m also working on getting into good physical shape, although I had a set back with a broken hip. The softness of my bones is largely due to my 12 years of cancer treatments, which required me to have loads of steroids.
I have other fundraising plans, too, specifically for immunotherapies. Cancer patients have such a tough road as is, and then it’s worsened based on your financial situation and the quality of your health insurance and your geographic location. For such a wealthy society, it’s really sad how hard patients have to fight for access to medications. The barriers you can face with a life-threatening illness…it’s a real tragedy in our country.


They couldn’t believe what I had gone through
Through my advocacy work, I’ve had some amazing opportunities to meet scientists, including the guy who founded the CAR-T company that manufactured my treatment. I was able to thank him in person, and we filmed him for the documentary I’m working on. He said, "Laurie, if it wasn’t for patients like you who actually agreed to do this trial, we wouldn’t be here." And I said, "But I had no other option. I was dead otherwise. I had no choice." He replied, “I know, but you still went through a lot and without you, we wouldn't have learned how to handle side effects.” I also had the chance to share my story with hundreds of employees from his company. Many of them cried. "We never hear patient stories,” they said. They couldn’t believe what I had gone through.
I’m Laurie, and I’m 64 years old. I grew up in the Northeast, went to a small liberal arts college in upstate New York, and worked at a bank in Boston after graduation. In 1984, I accepted a job offer in Los Angeles. I packed up, moved west, and worked for a small startup software company. The transition was hard; LA can be a very lonely city if you don't have an established network. But I threw myself into my work. For a few years, I was bicoastal: two weeks in Manhattan and two weeks in LA. I had an apartment in both cities.
Before cancer, I was enjoying life, although my priority was always my career. I married late, had my son at 40, and had a successful, longtime career in financial services. I worked for the same company for nearly 25 years and eventually became president of the firm. I had a great run. But my job back then was to help other people make money. I was constantly working on the next thing: the next business product, the next market, the next board meeting. I was traveling internationally regularly. That said, after a 12-year, life-threatening cancer journey, I never went back to financial services. It held no appeal anymore. I had a rude, sudden awakening that I needed to stay focused on my health and help other cancer patients on their journeys.
A couple years after my diagnosis, it was clear the cancer wasn’t retreating and I needed to leave my work. When I stopped working, my son was going into third grade. I approached his teacher, shared my cancer journey, and offered to help in the classroom every morning, doing tasks like sharpening pencils and checking homework. It was weird (and I like to think nice) for my son to see me present every day, a stark contrast to my previous absence. But the blinders came off and I realized my priorities had been seriously misplaced.

I was dismissed by doctors for a good two years
It all started when I was 43 and experiencing frequent sinus infections. New symptoms kept appearing, including a very dry eye. I had been a contact lens wearer for 30 years and suddenly I couldn’t wear them anymore. I felt exhausted and had a gut feeling that something was very wrong. I went to a few doctors and they blamed hormones and allergies. I had an enlarged lymph node in my neck, and for that, they blamed sinus infections. As to the lump I felt in my abdomen, they said it was likely a hernia. Part of me really wanted to believe they were right and that nothing was wrong. But I just knew the doctors were wrong. I eventually took my husband to some of my appointments; he was shocked at the way the doctors treated me.
In the Spring of 2006, I went to “the best” ear, nose, and throat doctor in Los Angeles (I roll my eyes when I say this now as I know there is no such thing). I had done a Google search of my symptoms (as one does, right?) and was worried that my sinus infections were related to lymphoma. My husband joined me for the consult, as I felt his being there would be helpful. When I shared my symptoms with the doctor and said I was worried I might have lymphoma, he looked at my husband and rolled his eyes as if I were some stupid blonde. He then looked at me and said, “How did you even come up with that idea?” I replied, “The Internet.” He went, “Ah, Dr. Google. Well, I went to Med school for 12 years and did a residency plus a fellowship.” He looked at my husband and rolled his eyes again. It was infuriating, just unbelievable. He then said, “You don’t have lymphoma. If you let me treat you for your allergies, you’re going to be fine.” I replied, “Doctor, that’s all fine and good, but I got tested for allergies and I don’t have any allergies. I’ve never had allergies.”
I shared with him that I also was really fatigued all the time. Once again, he rolled his eyes and said, “Well, what do you think that could be from? You're running a company, traveling to London and New York regularly, all while running a household with a little kid at home. I'm tired just listening to you. Your blood work is all normal. You're fine. You just have allergies."
I wanted to believe him, but in my heart, I knew.
I wanted to get another opinion, so I called an old friend in LA and asked if she knew a diagnostician. She recommended someone nearby and a couple weeks later, I saw him. He agreed that it could be a hernia, sinus issues, hormonal changes, or dry eyes. “But we don’t make guesses about this stuff. That’s why we have CT machines,” he said. Out of the many doctors I had seen, he was the first to order a CT of my abdomen to confirm it was a hernia. Two days after the CT, I received a call and was told I needed to come in that same day, which happened to be Good Friday in 2006. My son was in kindergarten at the time of my diagnosis. I learned I had either a mesenchymal tumor that would likely be fatal within 30 days, or some kind of lymphoma. He made an appointment for me with an oncologist for the following Monday at an oncology practice. I said, “I can’t go on Monday. I have to fly to New York and Chicago because I’m having my annual client conferences. We have 300 of our clients coming and I’m giving the keynote speech.” He looked at me like I was a bit crazy but told me fine, and that as soon as I was back, I’d need to get on it right away.
We continued talking and suddenly, it all hit me. I said, “I guess I’m not going to New York and Chicago, am I?” He replied, “I certainly hope not.”
I wanted to be anybody but me
I had the PET-CT that Monday. I remember being in the car as my husband drove me to the appointment. I saw a sanitation worker emptying a trash can and wished I could switch places with him. I wanted to be anybody but me. My body had completely let me down. I thought, “How could this happen to me?” I had never smoked or engaged in cancer-causing activities. Where had I gone wrong? I was trying so hard to point fingers at myself. But I quickly learned it can all just be random. And it’s not your fault.
The scans confirmed I had stage 4 follicular Non Hodgkin's lymphoma. They said given the size of the tumor, I had likely had it for at least five years, meaning I could have had it when I was pregnant with my son. So that “hernia” in my abdomen I had told my doctor about? It was, in fact, a giant metastasized tumor the size of a grapefruit. And the dry eye? That was because I had a tumor blocking my tear duct.
It was cancer the entire time. But no one believed me.
One of the first things I did was write a letter to the ENT doctor who ignored me. “I was the blonde lady who came in concerned she had lymphoma. You were completely dismissive and insulting. You rolled your eyes at my husband when I asked if I had lymphoma. I just learned that in fact I do have lymphoma and it’s stage 4. I hope the next time a patient comes in, you won’t roll your eyes at them and dismiss their concerns. Listen to them. Listen to your patient.”
It felt good writing that letter. I was never going to take action - I wasn’t going to file a suit - but maybe I raised his awareness a bit.
I remember not knowing whether I should even tell my son I was sick. But my oncologist said, “You're going to lose your hair from the chemo. If you don’t tell him, he’ll go to school, tell his friends his mom lost her hair, and they’ll say something like ‘Oh, that happened to my grandma too. She died from cancer.’ I realized I needed to get in front of it, so we told my son right away. He said, “But Mommy, girls aren’t bald!” But then he said, "Oh, wait, you're gonna be bald, Mommy…COOL”!" The way he said it…it was as if it was the coolest thing in the world. It was really sweet. But it was also really hard. That same night my husband and I told him about my illness, my son called me into his room after lights out. He said, "Mommy, will you come in here because I'm really worried." I said, "What's the matter?" And he said, "You're going to be bald. Is everybody going to make fun of you?" I said, "Oh, no, I will wear a wig, scarf and hats. Nobody's going to know. Don't worry, it will be fine. And when my hair starts to fall out, you can help me pull it out and we’ll donate it."
My son had a mom who had an incurable cancer and was in treatment for his entire childhood – his elementary, middle and high school years. He grew up fast. Even when he was young, he really stepped up. Of course he couldn't drive or go to the market and get groceries, but he could give me lots of love. He could climb into bed and hug me. He helped as much as he could around the house. I remember when he was in kindergarten, I told him that talking to someone about his feelings might help him feel better. But he insisted, "No, Mommy, I'm fine. I have to take care of you."
I had to start treatment right away because I was so sick and symptomatic
There was one approved treatment back in 2006, which was a chemo monoclonal antibody combination (the “big guns” as they called it). I started treatment in May of 2006 and took leave from my firm. On September 11, I had my sixth and final treatment. They scanned me and my disease was gone. I was told that since my disease responded so quickly, I would likely have a durable remission. I went back to work shortly after and resumed my crazy schedule and traveling. When I traveled, I wore a mask to keep other’s germs away from me, as the chemo had depleted my immune system – I think I was ahead of my time on the mask thing!
I received maintenance treatment every three months. In January the next year, they scanned me again and found out there was activity in my lungs. They said it could just be inflammation, but they recommended I see a pulmonologist and a lung surgeon. A lung biopsy is a really difficult thing to do, so we decided to just watch and wait, and gradually the disease was large enough that I had to find a new treatment.
When I was first diagnosed, I got four opinions. I’m lucky I live in LA because there are a lot of cancer hospitals. I made my rounds and they all agreed that if the chemo didn’t work, the next option would be an autologous stem cell transplant (SCT) with my own cells. So later on when my cancer came back after chemo, we had already harvested my stem cells as an insurance policy, should I ever need a transplant. But it’s a very difficult process and would require I get more brute force chemo. I also would be in the hospital for a month. I had done my own research on auto SCT and found that half of patients with my diagnosis relapsed in less than a year after a stem cell transplant. And, if you failed the type of chemo I had (which I did), the chances of durable remission after a stem cell transplant were very low.
I told the oncologist at the transplant center that I couldn’t do an SCT. I said, “I have a little kid at home. I can’t go to the hospital for a month. If it was a 90% chance of complete remission, then we’d make it work but at less than a 50% chance of durable remission, I just can’t do it. The odds for me just stink.”
He said to me, “Laurie, I’m going to find you a clinical trial.”
So I started my first clinical trial and while it didn’t shrink the tumor, it did stabilize it. I got a scan every three months and as long as you have a stable or smaller disease, you can continue on the trial. I felt so well-cared for in the trial as opposed to chemo, where I really felt like I was on my own. When I first enrolled, I was assigned a trial coordinator who efficiently organized all my appointments, biopsies, scans, and treatments. This made the process much more manageable. They provided continuous support and proactively checked in with me several times a week. From that point on, I was sold on clinical trials and convinced they would be part of my survival.
It felt like a death sentence
At my nine-month scan during that first clinical trial, my tumor had shrunk a little bit. My oncologist said, “Wow, this is a win. It’s shrinking. It’s working.” But at my one-year scan, it had grown. I was ousted from the trial. That said, in that one year period, new treatments had been approved, so I was given a new chemotherapy. This was my third line of treatment. I did chemo once a month for an entire year. My disease got smaller, but it was still present. We followed it up with a fourth treatment: radioimmunotherapy, which had just been approved. I spoke with patients who had been in the clinical trial for it; they were 10 years out and had complete remission. I thought to myself, “Treatment 4 will be different.” I thought for sure it was going to work.
A couple months after the radioimmunotherapy, I was reading and felt a tumor in the back of my neck. My cancer was back, and again, it was everywhere. It was as if the radioimmunotherapy had done nothing. My oncologist said the only option I had left was an allogeneic stem cell transplant, where you would get a new immune system from a donor. I saw multiple doctors and they all said the same thing: allo transplant. The patient gets more chemo to destroy the cancer, but it also destroys your immune system. Once the patient is in complete remission from the chemo, a donor’s stem cells are infused into you. It’s very risky. Many patients don’t make it out of the hospital. And the more heavily treated you are (like I was) the more likely you are to have problems.
The best donor is a sibling but neither of my two siblings were matches, so we looked into donor banks and discovered I had many matches - good news. But when you receive a donor’s stem cells and immune system, you can develop what's called graft versus host disease, where your new immune system starts to attack your existing organs. Doctors put patients on immune suppressors to minimize the risk, but this can lead to secondary cancer. The option of allo SCT terrified me.
It's an unbelievable story
I emailed a good friend of mine, letting her know I had relapsed again. She called me and said, “What are you doing right now?” I said, “I'm going to bed, I'm so depressed. I have to get up at three to pick up my son at school. But in the meantime, I'm going to bed.” She said, “No you're not. You’re going to turn your computer on, I'm going to come over, and we're going to find you another clinical trial. You are not going to do an allogeneic stem cell transplant.” She came over, we researched and found eight trials inside and outside the US - including one nearby at UCLA - and emailed the lead investigators for each. My friend left, I went back to bed, and an hour later my telephone rang. I looked at the caller ID and it said UCLA. I answered. “Laurie, this is the lead investigator at UCLA. I just read your email. I have a clinical trial that I think would work really well for you.” I immediately said, “But I'm so heavily treated and this will be my fifth line of therapy, why do you think it will work?” He said, “Because this drug is helping patients exactly like you who are heavily treated. Nothing else has worked for these patients, even those who’ve had transplants. But this is working for them. But I need you to come in today because it's a phase one trial, I have 19 people enrolled so far and I only have one spot left.”
I was supposed to attend and help set up a fundraiser that night for a non-profit blood cancer organization. I shared that with the oncologist, and coincidentally, he was also attending. We met that night at the event, and I reviewed and signed the trial paperwork. It's an unbelievable story - if my friend hadn’t insisted on coming over that day, none of this would have happened.
The trial was Phase 1 and it was testing a small molecule drug, a PI3 kinase inhibitor. The treatment was a pill I took in the morning and at night. Within days, my tumors were shrinking. I ended up being the “long tail” on that trial, which means I was the patient who was on the trial the longest. I was on the drug for almost six years – from spring 2011 until December 31, 2016. It had a GI side effect and it never put me in a complete remission, but it kept my disease stable and bought me loads of time for better options to come along.
It was a race against time for CAR-T Therapy
At the end of 2016, my cancer relapsed and I was removed from the Pi3 Kinase inhibitor trial. At that point, there was a new monoclonal antibody that had been approved, so I did that for 10 months and the tumor started to shrink and stabilize again. But as soon as I stopped that treatment, the cancer returned. I was in a race against time, hoping an immunotherapy called CAR-T cell therapy would become available in time to save my life. I had heard about CAR-T in 2012, but it wasn’t being tested for follicular NHL yet.
In Spring 2018, I got the call from my oncologist. “The CAR-T for fNHL trial is opening at UCLA. You will be the first of five patients to enroll.” I got the treatment July 16 and 30 days later, my cancer was completely gone and I was finally in a complete remission. The before and after scans were unbelievable…an estimated 8 pounds of tumor vanished as a result of CAR-T. I am now 6 years in complete remission post CAR-T. Follicular non-Hodgkin lymphoma has always been considered incurable, but my oncologist believes I'm cured. He said, “Laurie, you're done with lymphoma. Thanks to CAR-T, this cancer now has a cure.”
My little boy was my biggest motivator
I relapsed six times over the course of 12 years and was in continuous treatment all those years. People ask me, “Laurie, how did you do this? How did you keep going?” My motivator was my little boy. The thought of my husband having to tell my son that mommy died…it was just unfathomable. I said, I cannot let that happen. I have to fight. And if something doesn’t work, I have to find the next thing. I don't care what I have to do. I am not dying. My husband said, “What about me?” Of course I did not want to leave my husband either, but reminded him “You can get another wife, but our son cannot get another mom.”
Those 12 years felt like a roller coaster. Every time I would get optimistic, I’d get slammed down again. But I’d pick myself back up, brush myself off, and tell myself, “Find the next treatment, maybe it will work.” I vividly remember picking my son up from school when he was in the First Grade. I’d be waiting at the picnic bench when the class door would open and out he would run to me and jump into my arms. I’d say to myself, “I can’t miss these moments. I have to find the next treatment.”
I know I’m biased because I'm his mom, but my son was always caring and responsible. He worked multiple jobs starting at age 13. He delivered newspapers, had lemonade stands, and was a junior lifeguard and a skate guard at a local ice rink. Choosing a college was very tough for him: stay in LA or go away. We encouraged him to go away. It was hard for him after watching me fight my cancer, a cancer diagnosis impacts everyone in your life. So my son flew across the country to have his college experience. The summer I received CAR-T, he was certified as an EMT so could volunteer during his college years.
My husband and I have been together now for 30 years. During my cancer fight, I was strong and tried to keep my husband and my son out of everything as much as I could. My husband had a business to run, and I wanted him to focus on that while I dealt with the cancer. He used to say, "You're going to outlive me, you're so tuned in with all the medical details."

Swimming was my meditation
I found out early in my treatment that I needed to be active physically, mostly because I was a wreck emotionally. I was depressed and anxious. One day after a chemo treatment I said, "When I get home, I'm going to put on my tennis shoes, and I'm just going to walk to the end of the street." So I did that, and when I got back I thought, "That was really good." Not long after that, I started swimming. I had been taking my son to swim lessons at a local community college pool in Santa Monica. One day while he was in his lesson, I thought, "I'm going to go to the adult pool. I'm going to try to swim laps." I was still doing chemo and it was summer, so it was hot. Walking was hard because I’d get dizzy in the heat. So the pool seemed like a good alternative. I remember that first day I swam nearly 20 laps. It felt so great. It was slow - just like the walking - but it really helped me emotionally. I’ve never been able to meditate or do yoga. I’ve tried, but they’re just not for me. Lap swimming became my moving meditation.
I also went on an antidepressant. I felt like I needed to do everything I could to get my head working with my body. Day to day tasks at times were both physically and mentally challenging. I remember one time, a man walked up to me in the grocery store. I was wearing a scarf and he said “Oh, you must be doing chemo. How can you put that toxic stuff in your body, it will kill you! You just need a macrobiotic diet and you’ll be fine.” There was a woman in line, right in front of me, and she chimed in saying “Excuse me, what did you just say?” She reprimanded him. It turned out she was a survivor.
This experience has changed my life’s mission
Raising awareness of the game changing CAR-T immunotherapy and the benefit of clinical trials is my work now. People think of clinical trials from the scary stories of old. I was an early convert to clinical trials. Three of the seven treatments I had in my 12-year journey were clinical trials, and all three were provided at no cost to me. I learned quickly that clinical trials are often much smarter than standard of care therapies, they are more targeted and typically have fewer side effects. I’m a huge advocate for education around clinical trials.
There are access issues. Living in LA, I had access to multiple cancer centers for treatments and trials. During my 12-year journey, I was treated at four large cancer centers in Los Angeles. But many people are lucky if they have just one place in their state where they can access a trial. I’m trying to help change this. I work as a volunteer legislative advocate for the Leukemia & Lymphoma Society at both state and federal levels, to help make laws that require pharmaceutical companies to have more diversity in trials (racially, ethnically, geographically, and socioeconomically). I also work on advocating for patients and raising awareness of newer therapies, such as immunotherapies, which are more targeted. If you’re being treated at a community oncology center with an oncology generalist, they’re likely going to be doing what they’ve been doing for the past 30 years, which is chemo, transplant, and more chemo. They can’t possibly keep up to speed with all of the newer developments. I was an advocate for myself and I pushed and I pushed and I pushed. But not all patients can do that. Some aren’t equipped to be their own advocates due to language barriers, and some don’t have caregivers to help them. There are so many barriers, and because of that, we don’t have nearly enough diversity in clinical trials.
Cancer patients have such a tough road
I now spend about 20 hours a week as a cancer volunteer advocate for three different nonprofits. Helping others navigate their cancer journeys is something I am adept at. I’m also working on getting into good physical shape, although I had a set back with a broken hip. The softness of my bones is largely due to my 12 years of cancer treatments, which required me to have loads of steroids.
I have other fundraising plans, too, specifically for immunotherapies. Cancer patients have such a tough road as is, and then it’s worsened based on your financial situation and the quality of your health insurance and your geographic location. For such a wealthy society, it’s really sad how hard patients have to fight for access to medications. The barriers you can face with a life-threatening illness…it’s a real tragedy in our country.


They couldn’t believe what I had gone through
Through my advocacy work, I’ve had some amazing opportunities to meet scientists, including the guy who founded the CAR-T company that manufactured my treatment. I was able to thank him in person, and we filmed him for the documentary I’m working on. He said, "Laurie, if it wasn’t for patients like you who actually agreed to do this trial, we wouldn’t be here." And I said, "But I had no other option. I was dead otherwise. I had no choice." He replied, “I know, but you still went through a lot and without you, we wouldn't have learned how to handle side effects.” I also had the chance to share my story with hundreds of employees from his company. Many of them cried. "We never hear patient stories,” they said. They couldn’t believe what I had gone through.
I’m Laurie, and I’m 64 years old. I grew up in the Northeast, went to a small liberal arts college in upstate New York, and worked at a bank in Boston after graduation. In 1984, I accepted a job offer in Los Angeles. I packed up, moved west, and worked for a small startup software company. The transition was hard; LA can be a very lonely city if you don't have an established network. But I threw myself into my work. For a few years, I was bicoastal: two weeks in Manhattan and two weeks in LA. I had an apartment in both cities.
Before cancer, I was enjoying life, although my priority was always my career. I married late, had my son at 40, and had a successful, longtime career in financial services. I worked for the same company for nearly 25 years and eventually became president of the firm. I had a great run. But my job back then was to help other people make money. I was constantly working on the next thing: the next business product, the next market, the next board meeting. I was traveling internationally regularly. That said, after a 12-year, life-threatening cancer journey, I never went back to financial services. It held no appeal anymore. I had a rude, sudden awakening that I needed to stay focused on my health and help other cancer patients on their journeys.
A couple years after my diagnosis, it was clear the cancer wasn’t retreating and I needed to leave my work. When I stopped working, my son was going into third grade. I approached his teacher, shared my cancer journey, and offered to help in the classroom every morning, doing tasks like sharpening pencils and checking homework. It was weird (and I like to think nice) for my son to see me present every day, a stark contrast to my previous absence. But the blinders came off and I realized my priorities had been seriously misplaced.

I was dismissed by doctors for a good two years
It all started when I was 43 and experiencing frequent sinus infections. New symptoms kept appearing, including a very dry eye. I had been a contact lens wearer for 30 years and suddenly I couldn’t wear them anymore. I felt exhausted and had a gut feeling that something was very wrong. I went to a few doctors and they blamed hormones and allergies. I had an enlarged lymph node in my neck, and for that, they blamed sinus infections. As to the lump I felt in my abdomen, they said it was likely a hernia. Part of me really wanted to believe they were right and that nothing was wrong. But I just knew the doctors were wrong. I eventually took my husband to some of my appointments; he was shocked at the way the doctors treated me.
In the Spring of 2006, I went to “the best” ear, nose, and throat doctor in Los Angeles (I roll my eyes when I say this now as I know there is no such thing). I had done a Google search of my symptoms (as one does, right?) and was worried that my sinus infections were related to lymphoma. My husband joined me for the consult, as I felt his being there would be helpful. When I shared my symptoms with the doctor and said I was worried I might have lymphoma, he looked at my husband and rolled his eyes as if I were some stupid blonde. He then looked at me and said, “How did you even come up with that idea?” I replied, “The Internet.” He went, “Ah, Dr. Google. Well, I went to Med school for 12 years and did a residency plus a fellowship.” He looked at my husband and rolled his eyes again. It was infuriating, just unbelievable. He then said, “You don’t have lymphoma. If you let me treat you for your allergies, you’re going to be fine.” I replied, “Doctor, that’s all fine and good, but I got tested for allergies and I don’t have any allergies. I’ve never had allergies.”
I shared with him that I also was really fatigued all the time. Once again, he rolled his eyes and said, “Well, what do you think that could be from? You're running a company, traveling to London and New York regularly, all while running a household with a little kid at home. I'm tired just listening to you. Your blood work is all normal. You're fine. You just have allergies."
I wanted to believe him, but in my heart, I knew.
I wanted to get another opinion, so I called an old friend in LA and asked if she knew a diagnostician. She recommended someone nearby and a couple weeks later, I saw him. He agreed that it could be a hernia, sinus issues, hormonal changes, or dry eyes. “But we don’t make guesses about this stuff. That’s why we have CT machines,” he said. Out of the many doctors I had seen, he was the first to order a CT of my abdomen to confirm it was a hernia. Two days after the CT, I received a call and was told I needed to come in that same day, which happened to be Good Friday in 2006. My son was in kindergarten at the time of my diagnosis. I learned I had either a mesenchymal tumor that would likely be fatal within 30 days, or some kind of lymphoma. He made an appointment for me with an oncologist for the following Monday at an oncology practice. I said, “I can’t go on Monday. I have to fly to New York and Chicago because I’m having my annual client conferences. We have 300 of our clients coming and I’m giving the keynote speech.” He looked at me like I was a bit crazy but told me fine, and that as soon as I was back, I’d need to get on it right away.
We continued talking and suddenly, it all hit me. I said, “I guess I’m not going to New York and Chicago, am I?” He replied, “I certainly hope not.”
I wanted to be anybody but me
I had the PET-CT that Monday. I remember being in the car as my husband drove me to the appointment. I saw a sanitation worker emptying a trash can and wished I could switch places with him. I wanted to be anybody but me. My body had completely let me down. I thought, “How could this happen to me?” I had never smoked or engaged in cancer-causing activities. Where had I gone wrong? I was trying so hard to point fingers at myself. But I quickly learned it can all just be random. And it’s not your fault.
The scans confirmed I had stage 4 follicular Non Hodgkin's lymphoma. They said given the size of the tumor, I had likely had it for at least five years, meaning I could have had it when I was pregnant with my son. So that “hernia” in my abdomen I had told my doctor about? It was, in fact, a giant metastasized tumor the size of a grapefruit. And the dry eye? That was because I had a tumor blocking my tear duct.
It was cancer the entire time. But no one believed me.
One of the first things I did was write a letter to the ENT doctor who ignored me. “I was the blonde lady who came in concerned she had lymphoma. You were completely dismissive and insulting. You rolled your eyes at my husband when I asked if I had lymphoma. I just learned that in fact I do have lymphoma and it’s stage 4. I hope the next time a patient comes in, you won’t roll your eyes at them and dismiss their concerns. Listen to them. Listen to your patient.”
It felt good writing that letter. I was never going to take action - I wasn’t going to file a suit - but maybe I raised his awareness a bit.
I remember not knowing whether I should even tell my son I was sick. But my oncologist said, “You're going to lose your hair from the chemo. If you don’t tell him, he’ll go to school, tell his friends his mom lost her hair, and they’ll say something like ‘Oh, that happened to my grandma too. She died from cancer.’ I realized I needed to get in front of it, so we told my son right away. He said, “But Mommy, girls aren’t bald!” But then he said, "Oh, wait, you're gonna be bald, Mommy…COOL”!" The way he said it…it was as if it was the coolest thing in the world. It was really sweet. But it was also really hard. That same night my husband and I told him about my illness, my son called me into his room after lights out. He said, "Mommy, will you come in here because I'm really worried." I said, "What's the matter?" And he said, "You're going to be bald. Is everybody going to make fun of you?" I said, "Oh, no, I will wear a wig, scarf and hats. Nobody's going to know. Don't worry, it will be fine. And when my hair starts to fall out, you can help me pull it out and we’ll donate it."
My son had a mom who had an incurable cancer and was in treatment for his entire childhood – his elementary, middle and high school years. He grew up fast. Even when he was young, he really stepped up. Of course he couldn't drive or go to the market and get groceries, but he could give me lots of love. He could climb into bed and hug me. He helped as much as he could around the house. I remember when he was in kindergarten, I told him that talking to someone about his feelings might help him feel better. But he insisted, "No, Mommy, I'm fine. I have to take care of you."
I had to start treatment right away because I was so sick and symptomatic
There was one approved treatment back in 2006, which was a chemo monoclonal antibody combination (the “big guns” as they called it). I started treatment in May of 2006 and took leave from my firm. On September 11, I had my sixth and final treatment. They scanned me and my disease was gone. I was told that since my disease responded so quickly, I would likely have a durable remission. I went back to work shortly after and resumed my crazy schedule and traveling. When I traveled, I wore a mask to keep other’s germs away from me, as the chemo had depleted my immune system – I think I was ahead of my time on the mask thing!
I received maintenance treatment every three months. In January the next year, they scanned me again and found out there was activity in my lungs. They said it could just be inflammation, but they recommended I see a pulmonologist and a lung surgeon. A lung biopsy is a really difficult thing to do, so we decided to just watch and wait, and gradually the disease was large enough that I had to find a new treatment.
When I was first diagnosed, I got four opinions. I’m lucky I live in LA because there are a lot of cancer hospitals. I made my rounds and they all agreed that if the chemo didn’t work, the next option would be an autologous stem cell transplant (SCT) with my own cells. So later on when my cancer came back after chemo, we had already harvested my stem cells as an insurance policy, should I ever need a transplant. But it’s a very difficult process and would require I get more brute force chemo. I also would be in the hospital for a month. I had done my own research on auto SCT and found that half of patients with my diagnosis relapsed in less than a year after a stem cell transplant. And, if you failed the type of chemo I had (which I did), the chances of durable remission after a stem cell transplant were very low.
I told the oncologist at the transplant center that I couldn’t do an SCT. I said, “I have a little kid at home. I can’t go to the hospital for a month. If it was a 90% chance of complete remission, then we’d make it work but at less than a 50% chance of durable remission, I just can’t do it. The odds for me just stink.”
He said to me, “Laurie, I’m going to find you a clinical trial.”
So I started my first clinical trial and while it didn’t shrink the tumor, it did stabilize it. I got a scan every three months and as long as you have a stable or smaller disease, you can continue on the trial. I felt so well-cared for in the trial as opposed to chemo, where I really felt like I was on my own. When I first enrolled, I was assigned a trial coordinator who efficiently organized all my appointments, biopsies, scans, and treatments. This made the process much more manageable. They provided continuous support and proactively checked in with me several times a week. From that point on, I was sold on clinical trials and convinced they would be part of my survival.
It felt like a death sentence
At my nine-month scan during that first clinical trial, my tumor had shrunk a little bit. My oncologist said, “Wow, this is a win. It’s shrinking. It’s working.” But at my one-year scan, it had grown. I was ousted from the trial. That said, in that one year period, new treatments had been approved, so I was given a new chemotherapy. This was my third line of treatment. I did chemo once a month for an entire year. My disease got smaller, but it was still present. We followed it up with a fourth treatment: radioimmunotherapy, which had just been approved. I spoke with patients who had been in the clinical trial for it; they were 10 years out and had complete remission. I thought to myself, “Treatment 4 will be different.” I thought for sure it was going to work.
A couple months after the radioimmunotherapy, I was reading and felt a tumor in the back of my neck. My cancer was back, and again, it was everywhere. It was as if the radioimmunotherapy had done nothing. My oncologist said the only option I had left was an allogeneic stem cell transplant, where you would get a new immune system from a donor. I saw multiple doctors and they all said the same thing: allo transplant. The patient gets more chemo to destroy the cancer, but it also destroys your immune system. Once the patient is in complete remission from the chemo, a donor’s stem cells are infused into you. It’s very risky. Many patients don’t make it out of the hospital. And the more heavily treated you are (like I was) the more likely you are to have problems.
The best donor is a sibling but neither of my two siblings were matches, so we looked into donor banks and discovered I had many matches - good news. But when you receive a donor’s stem cells and immune system, you can develop what's called graft versus host disease, where your new immune system starts to attack your existing organs. Doctors put patients on immune suppressors to minimize the risk, but this can lead to secondary cancer. The option of allo SCT terrified me.
It's an unbelievable story
I emailed a good friend of mine, letting her know I had relapsed again. She called me and said, “What are you doing right now?” I said, “I'm going to bed, I'm so depressed. I have to get up at three to pick up my son at school. But in the meantime, I'm going to bed.” She said, “No you're not. You’re going to turn your computer on, I'm going to come over, and we're going to find you another clinical trial. You are not going to do an allogeneic stem cell transplant.” She came over, we researched and found eight trials inside and outside the US - including one nearby at UCLA - and emailed the lead investigators for each. My friend left, I went back to bed, and an hour later my telephone rang. I looked at the caller ID and it said UCLA. I answered. “Laurie, this is the lead investigator at UCLA. I just read your email. I have a clinical trial that I think would work really well for you.” I immediately said, “But I'm so heavily treated and this will be my fifth line of therapy, why do you think it will work?” He said, “Because this drug is helping patients exactly like you who are heavily treated. Nothing else has worked for these patients, even those who’ve had transplants. But this is working for them. But I need you to come in today because it's a phase one trial, I have 19 people enrolled so far and I only have one spot left.”
I was supposed to attend and help set up a fundraiser that night for a non-profit blood cancer organization. I shared that with the oncologist, and coincidentally, he was also attending. We met that night at the event, and I reviewed and signed the trial paperwork. It's an unbelievable story - if my friend hadn’t insisted on coming over that day, none of this would have happened.
The trial was Phase 1 and it was testing a small molecule drug, a PI3 kinase inhibitor. The treatment was a pill I took in the morning and at night. Within days, my tumors were shrinking. I ended up being the “long tail” on that trial, which means I was the patient who was on the trial the longest. I was on the drug for almost six years – from spring 2011 until December 31, 2016. It had a GI side effect and it never put me in a complete remission, but it kept my disease stable and bought me loads of time for better options to come along.
It was a race against time for CAR-T Therapy
At the end of 2016, my cancer relapsed and I was removed from the Pi3 Kinase inhibitor trial. At that point, there was a new monoclonal antibody that had been approved, so I did that for 10 months and the tumor started to shrink and stabilize again. But as soon as I stopped that treatment, the cancer returned. I was in a race against time, hoping an immunotherapy called CAR-T cell therapy would become available in time to save my life. I had heard about CAR-T in 2012, but it wasn’t being tested for follicular NHL yet.
In Spring 2018, I got the call from my oncologist. “The CAR-T for fNHL trial is opening at UCLA. You will be the first of five patients to enroll.” I got the treatment July 16 and 30 days later, my cancer was completely gone and I was finally in a complete remission. The before and after scans were unbelievable…an estimated 8 pounds of tumor vanished as a result of CAR-T. I am now 6 years in complete remission post CAR-T. Follicular non-Hodgkin lymphoma has always been considered incurable, but my oncologist believes I'm cured. He said, “Laurie, you're done with lymphoma. Thanks to CAR-T, this cancer now has a cure.”
My little boy was my biggest motivator
I relapsed six times over the course of 12 years and was in continuous treatment all those years. People ask me, “Laurie, how did you do this? How did you keep going?” My motivator was my little boy. The thought of my husband having to tell my son that mommy died…it was just unfathomable. I said, I cannot let that happen. I have to fight. And if something doesn’t work, I have to find the next thing. I don't care what I have to do. I am not dying. My husband said, “What about me?” Of course I did not want to leave my husband either, but reminded him “You can get another wife, but our son cannot get another mom.”
Those 12 years felt like a roller coaster. Every time I would get optimistic, I’d get slammed down again. But I’d pick myself back up, brush myself off, and tell myself, “Find the next treatment, maybe it will work.” I vividly remember picking my son up from school when he was in the First Grade. I’d be waiting at the picnic bench when the class door would open and out he would run to me and jump into my arms. I’d say to myself, “I can’t miss these moments. I have to find the next treatment.”
I know I’m biased because I'm his mom, but my son was always caring and responsible. He worked multiple jobs starting at age 13. He delivered newspapers, had lemonade stands, and was a junior lifeguard and a skate guard at a local ice rink. Choosing a college was very tough for him: stay in LA or go away. We encouraged him to go away. It was hard for him after watching me fight my cancer, a cancer diagnosis impacts everyone in your life. So my son flew across the country to have his college experience. The summer I received CAR-T, he was certified as an EMT so could volunteer during his college years.
My husband and I have been together now for 30 years. During my cancer fight, I was strong and tried to keep my husband and my son out of everything as much as I could. My husband had a business to run, and I wanted him to focus on that while I dealt with the cancer. He used to say, "You're going to outlive me, you're so tuned in with all the medical details."

Swimming was my meditation
I found out early in my treatment that I needed to be active physically, mostly because I was a wreck emotionally. I was depressed and anxious. One day after a chemo treatment I said, "When I get home, I'm going to put on my tennis shoes, and I'm just going to walk to the end of the street." So I did that, and when I got back I thought, "That was really good." Not long after that, I started swimming. I had been taking my son to swim lessons at a local community college pool in Santa Monica. One day while he was in his lesson, I thought, "I'm going to go to the adult pool. I'm going to try to swim laps." I was still doing chemo and it was summer, so it was hot. Walking was hard because I’d get dizzy in the heat. So the pool seemed like a good alternative. I remember that first day I swam nearly 20 laps. It felt so great. It was slow - just like the walking - but it really helped me emotionally. I’ve never been able to meditate or do yoga. I’ve tried, but they’re just not for me. Lap swimming became my moving meditation.
I also went on an antidepressant. I felt like I needed to do everything I could to get my head working with my body. Day to day tasks at times were both physically and mentally challenging. I remember one time, a man walked up to me in the grocery store. I was wearing a scarf and he said “Oh, you must be doing chemo. How can you put that toxic stuff in your body, it will kill you! You just need a macrobiotic diet and you’ll be fine.” There was a woman in line, right in front of me, and she chimed in saying “Excuse me, what did you just say?” She reprimanded him. It turned out she was a survivor.
This experience has changed my life’s mission
Raising awareness of the game changing CAR-T immunotherapy and the benefit of clinical trials is my work now. People think of clinical trials from the scary stories of old. I was an early convert to clinical trials. Three of the seven treatments I had in my 12-year journey were clinical trials, and all three were provided at no cost to me. I learned quickly that clinical trials are often much smarter than standard of care therapies, they are more targeted and typically have fewer side effects. I’m a huge advocate for education around clinical trials.
There are access issues. Living in LA, I had access to multiple cancer centers for treatments and trials. During my 12-year journey, I was treated at four large cancer centers in Los Angeles. But many people are lucky if they have just one place in their state where they can access a trial. I’m trying to help change this. I work as a volunteer legislative advocate for the Leukemia & Lymphoma Society at both state and federal levels, to help make laws that require pharmaceutical companies to have more diversity in trials (racially, ethnically, geographically, and socioeconomically). I also work on advocating for patients and raising awareness of newer therapies, such as immunotherapies, which are more targeted. If you’re being treated at a community oncology center with an oncology generalist, they’re likely going to be doing what they’ve been doing for the past 30 years, which is chemo, transplant, and more chemo. They can’t possibly keep up to speed with all of the newer developments. I was an advocate for myself and I pushed and I pushed and I pushed. But not all patients can do that. Some aren’t equipped to be their own advocates due to language barriers, and some don’t have caregivers to help them. There are so many barriers, and because of that, we don’t have nearly enough diversity in clinical trials.
Cancer patients have such a tough road
I now spend about 20 hours a week as a cancer volunteer advocate for three different nonprofits. Helping others navigate their cancer journeys is something I am adept at. I’m also working on getting into good physical shape, although I had a set back with a broken hip. The softness of my bones is largely due to my 12 years of cancer treatments, which required me to have loads of steroids.
I have other fundraising plans, too, specifically for immunotherapies. Cancer patients have such a tough road as is, and then it’s worsened based on your financial situation and the quality of your health insurance and your geographic location. For such a wealthy society, it’s really sad how hard patients have to fight for access to medications. The barriers you can face with a life-threatening illness…it’s a real tragedy in our country.


They couldn’t believe what I had gone through
Through my advocacy work, I’ve had some amazing opportunities to meet scientists, including the guy who founded the CAR-T company that manufactured my treatment. I was able to thank him in person, and we filmed him for the documentary I’m working on. He said, "Laurie, if it wasn’t for patients like you who actually agreed to do this trial, we wouldn’t be here." And I said, "But I had no other option. I was dead otherwise. I had no choice." He replied, “I know, but you still went through a lot and without you, we wouldn't have learned how to handle side effects.” I also had the chance to share my story with hundreds of employees from his company. Many of them cried. "We never hear patient stories,” they said. They couldn’t believe what I had gone through.
I’m Laurie, and I’m 64 years old. I grew up in the Northeast, went to a small liberal arts college in upstate New York, and worked at a bank in Boston after graduation. In 1984, I accepted a job offer in Los Angeles. I packed up, moved west, and worked for a small startup software company. The transition was hard; LA can be a very lonely city if you don't have an established network. But I threw myself into my work. For a few years, I was bicoastal: two weeks in Manhattan and two weeks in LA. I had an apartment in both cities.
Before cancer, I was enjoying life, although my priority was always my career. I married late, had my son at 40, and had a successful, longtime career in financial services. I worked for the same company for nearly 25 years and eventually became president of the firm. I had a great run. But my job back then was to help other people make money. I was constantly working on the next thing: the next business product, the next market, the next board meeting. I was traveling internationally regularly. That said, after a 12-year, life-threatening cancer journey, I never went back to financial services. It held no appeal anymore. I had a rude, sudden awakening that I needed to stay focused on my health and help other cancer patients on their journeys.
A couple years after my diagnosis, it was clear the cancer wasn’t retreating and I needed to leave my work. When I stopped working, my son was going into third grade. I approached his teacher, shared my cancer journey, and offered to help in the classroom every morning, doing tasks like sharpening pencils and checking homework. It was weird (and I like to think nice) for my son to see me present every day, a stark contrast to my previous absence. But the blinders came off and I realized my priorities had been seriously misplaced.

I was dismissed by doctors for a good two years
It all started when I was 43 and experiencing frequent sinus infections. New symptoms kept appearing, including a very dry eye. I had been a contact lens wearer for 30 years and suddenly I couldn’t wear them anymore. I felt exhausted and had a gut feeling that something was very wrong. I went to a few doctors and they blamed hormones and allergies. I had an enlarged lymph node in my neck, and for that, they blamed sinus infections. As to the lump I felt in my abdomen, they said it was likely a hernia. Part of me really wanted to believe they were right and that nothing was wrong. But I just knew the doctors were wrong. I eventually took my husband to some of my appointments; he was shocked at the way the doctors treated me.
In the Spring of 2006, I went to “the best” ear, nose, and throat doctor in Los Angeles (I roll my eyes when I say this now as I know there is no such thing). I had done a Google search of my symptoms (as one does, right?) and was worried that my sinus infections were related to lymphoma. My husband joined me for the consult, as I felt his being there would be helpful. When I shared my symptoms with the doctor and said I was worried I might have lymphoma, he looked at my husband and rolled his eyes as if I were some stupid blonde. He then looked at me and said, “How did you even come up with that idea?” I replied, “The Internet.” He went, “Ah, Dr. Google. Well, I went to Med school for 12 years and did a residency plus a fellowship.” He looked at my husband and rolled his eyes again. It was infuriating, just unbelievable. He then said, “You don’t have lymphoma. If you let me treat you for your allergies, you’re going to be fine.” I replied, “Doctor, that’s all fine and good, but I got tested for allergies and I don’t have any allergies. I’ve never had allergies.”
I shared with him that I also was really fatigued all the time. Once again, he rolled his eyes and said, “Well, what do you think that could be from? You're running a company, traveling to London and New York regularly, all while running a household with a little kid at home. I'm tired just listening to you. Your blood work is all normal. You're fine. You just have allergies."
I wanted to believe him, but in my heart, I knew.
I wanted to get another opinion, so I called an old friend in LA and asked if she knew a diagnostician. She recommended someone nearby and a couple weeks later, I saw him. He agreed that it could be a hernia, sinus issues, hormonal changes, or dry eyes. “But we don’t make guesses about this stuff. That’s why we have CT machines,” he said. Out of the many doctors I had seen, he was the first to order a CT of my abdomen to confirm it was a hernia. Two days after the CT, I received a call and was told I needed to come in that same day, which happened to be Good Friday in 2006. My son was in kindergarten at the time of my diagnosis. I learned I had either a mesenchymal tumor that would likely be fatal within 30 days, or some kind of lymphoma. He made an appointment for me with an oncologist for the following Monday at an oncology practice. I said, “I can’t go on Monday. I have to fly to New York and Chicago because I’m having my annual client conferences. We have 300 of our clients coming and I’m giving the keynote speech.” He looked at me like I was a bit crazy but told me fine, and that as soon as I was back, I’d need to get on it right away.
We continued talking and suddenly, it all hit me. I said, “I guess I’m not going to New York and Chicago, am I?” He replied, “I certainly hope not.”
I wanted to be anybody but me
I had the PET-CT that Monday. I remember being in the car as my husband drove me to the appointment. I saw a sanitation worker emptying a trash can and wished I could switch places with him. I wanted to be anybody but me. My body had completely let me down. I thought, “How could this happen to me?” I had never smoked or engaged in cancer-causing activities. Where had I gone wrong? I was trying so hard to point fingers at myself. But I quickly learned it can all just be random. And it’s not your fault.
The scans confirmed I had stage 4 follicular Non Hodgkin's lymphoma. They said given the size of the tumor, I had likely had it for at least five years, meaning I could have had it when I was pregnant with my son. So that “hernia” in my abdomen I had told my doctor about? It was, in fact, a giant metastasized tumor the size of a grapefruit. And the dry eye? That was because I had a tumor blocking my tear duct.
It was cancer the entire time. But no one believed me.
One of the first things I did was write a letter to the ENT doctor who ignored me. “I was the blonde lady who came in concerned she had lymphoma. You were completely dismissive and insulting. You rolled your eyes at my husband when I asked if I had lymphoma. I just learned that in fact I do have lymphoma and it’s stage 4. I hope the next time a patient comes in, you won’t roll your eyes at them and dismiss their concerns. Listen to them. Listen to your patient.”
It felt good writing that letter. I was never going to take action - I wasn’t going to file a suit - but maybe I raised his awareness a bit.
I remember not knowing whether I should even tell my son I was sick. But my oncologist said, “You're going to lose your hair from the chemo. If you don’t tell him, he’ll go to school, tell his friends his mom lost her hair, and they’ll say something like ‘Oh, that happened to my grandma too. She died from cancer.’ I realized I needed to get in front of it, so we told my son right away. He said, “But Mommy, girls aren’t bald!” But then he said, "Oh, wait, you're gonna be bald, Mommy…COOL”!" The way he said it…it was as if it was the coolest thing in the world. It was really sweet. But it was also really hard. That same night my husband and I told him about my illness, my son called me into his room after lights out. He said, "Mommy, will you come in here because I'm really worried." I said, "What's the matter?" And he said, "You're going to be bald. Is everybody going to make fun of you?" I said, "Oh, no, I will wear a wig, scarf and hats. Nobody's going to know. Don't worry, it will be fine. And when my hair starts to fall out, you can help me pull it out and we’ll donate it."
My son had a mom who had an incurable cancer and was in treatment for his entire childhood – his elementary, middle and high school years. He grew up fast. Even when he was young, he really stepped up. Of course he couldn't drive or go to the market and get groceries, but he could give me lots of love. He could climb into bed and hug me. He helped as much as he could around the house. I remember when he was in kindergarten, I told him that talking to someone about his feelings might help him feel better. But he insisted, "No, Mommy, I'm fine. I have to take care of you."
I had to start treatment right away because I was so sick and symptomatic
There was one approved treatment back in 2006, which was a chemo monoclonal antibody combination (the “big guns” as they called it). I started treatment in May of 2006 and took leave from my firm. On September 11, I had my sixth and final treatment. They scanned me and my disease was gone. I was told that since my disease responded so quickly, I would likely have a durable remission. I went back to work shortly after and resumed my crazy schedule and traveling. When I traveled, I wore a mask to keep other’s germs away from me, as the chemo had depleted my immune system – I think I was ahead of my time on the mask thing!
I received maintenance treatment every three months. In January the next year, they scanned me again and found out there was activity in my lungs. They said it could just be inflammation, but they recommended I see a pulmonologist and a lung surgeon. A lung biopsy is a really difficult thing to do, so we decided to just watch and wait, and gradually the disease was large enough that I had to find a new treatment.
When I was first diagnosed, I got four opinions. I’m lucky I live in LA because there are a lot of cancer hospitals. I made my rounds and they all agreed that if the chemo didn’t work, the next option would be an autologous stem cell transplant (SCT) with my own cells. So later on when my cancer came back after chemo, we had already harvested my stem cells as an insurance policy, should I ever need a transplant. But it’s a very difficult process and would require I get more brute force chemo. I also would be in the hospital for a month. I had done my own research on auto SCT and found that half of patients with my diagnosis relapsed in less than a year after a stem cell transplant. And, if you failed the type of chemo I had (which I did), the chances of durable remission after a stem cell transplant were very low.
I told the oncologist at the transplant center that I couldn’t do an SCT. I said, “I have a little kid at home. I can’t go to the hospital for a month. If it was a 90% chance of complete remission, then we’d make it work but at less than a 50% chance of durable remission, I just can’t do it. The odds for me just stink.”
He said to me, “Laurie, I’m going to find you a clinical trial.”
So I started my first clinical trial and while it didn’t shrink the tumor, it did stabilize it. I got a scan every three months and as long as you have a stable or smaller disease, you can continue on the trial. I felt so well-cared for in the trial as opposed to chemo, where I really felt like I was on my own. When I first enrolled, I was assigned a trial coordinator who efficiently organized all my appointments, biopsies, scans, and treatments. This made the process much more manageable. They provided continuous support and proactively checked in with me several times a week. From that point on, I was sold on clinical trials and convinced they would be part of my survival.
It felt like a death sentence
At my nine-month scan during that first clinical trial, my tumor had shrunk a little bit. My oncologist said, “Wow, this is a win. It’s shrinking. It’s working.” But at my one-year scan, it had grown. I was ousted from the trial. That said, in that one year period, new treatments had been approved, so I was given a new chemotherapy. This was my third line of treatment. I did chemo once a month for an entire year. My disease got smaller, but it was still present. We followed it up with a fourth treatment: radioimmunotherapy, which had just been approved. I spoke with patients who had been in the clinical trial for it; they were 10 years out and had complete remission. I thought to myself, “Treatment 4 will be different.” I thought for sure it was going to work.
A couple months after the radioimmunotherapy, I was reading and felt a tumor in the back of my neck. My cancer was back, and again, it was everywhere. It was as if the radioimmunotherapy had done nothing. My oncologist said the only option I had left was an allogeneic stem cell transplant, where you would get a new immune system from a donor. I saw multiple doctors and they all said the same thing: allo transplant. The patient gets more chemo to destroy the cancer, but it also destroys your immune system. Once the patient is in complete remission from the chemo, a donor’s stem cells are infused into you. It’s very risky. Many patients don’t make it out of the hospital. And the more heavily treated you are (like I was) the more likely you are to have problems.
The best donor is a sibling but neither of my two siblings were matches, so we looked into donor banks and discovered I had many matches - good news. But when you receive a donor’s stem cells and immune system, you can develop what's called graft versus host disease, where your new immune system starts to attack your existing organs. Doctors put patients on immune suppressors to minimize the risk, but this can lead to secondary cancer. The option of allo SCT terrified me.
It's an unbelievable story
I emailed a good friend of mine, letting her know I had relapsed again. She called me and said, “What are you doing right now?” I said, “I'm going to bed, I'm so depressed. I have to get up at three to pick up my son at school. But in the meantime, I'm going to bed.” She said, “No you're not. You’re going to turn your computer on, I'm going to come over, and we're going to find you another clinical trial. You are not going to do an allogeneic stem cell transplant.” She came over, we researched and found eight trials inside and outside the US - including one nearby at UCLA - and emailed the lead investigators for each. My friend left, I went back to bed, and an hour later my telephone rang. I looked at the caller ID and it said UCLA. I answered. “Laurie, this is the lead investigator at UCLA. I just read your email. I have a clinical trial that I think would work really well for you.” I immediately said, “But I'm so heavily treated and this will be my fifth line of therapy, why do you think it will work?” He said, “Because this drug is helping patients exactly like you who are heavily treated. Nothing else has worked for these patients, even those who’ve had transplants. But this is working for them. But I need you to come in today because it's a phase one trial, I have 19 people enrolled so far and I only have one spot left.”
I was supposed to attend and help set up a fundraiser that night for a non-profit blood cancer organization. I shared that with the oncologist, and coincidentally, he was also attending. We met that night at the event, and I reviewed and signed the trial paperwork. It's an unbelievable story - if my friend hadn’t insisted on coming over that day, none of this would have happened.
The trial was Phase 1 and it was testing a small molecule drug, a PI3 kinase inhibitor. The treatment was a pill I took in the morning and at night. Within days, my tumors were shrinking. I ended up being the “long tail” on that trial, which means I was the patient who was on the trial the longest. I was on the drug for almost six years – from spring 2011 until December 31, 2016. It had a GI side effect and it never put me in a complete remission, but it kept my disease stable and bought me loads of time for better options to come along.
It was a race against time for CAR-T Therapy
At the end of 2016, my cancer relapsed and I was removed from the Pi3 Kinase inhibitor trial. At that point, there was a new monoclonal antibody that had been approved, so I did that for 10 months and the tumor started to shrink and stabilize again. But as soon as I stopped that treatment, the cancer returned. I was in a race against time, hoping an immunotherapy called CAR-T cell therapy would become available in time to save my life. I had heard about CAR-T in 2012, but it wasn’t being tested for follicular NHL yet.
In Spring 2018, I got the call from my oncologist. “The CAR-T for fNHL trial is opening at UCLA. You will be the first of five patients to enroll.” I got the treatment July 16 and 30 days later, my cancer was completely gone and I was finally in a complete remission. The before and after scans were unbelievable…an estimated 8 pounds of tumor vanished as a result of CAR-T. I am now 6 years in complete remission post CAR-T. Follicular non-Hodgkin lymphoma has always been considered incurable, but my oncologist believes I'm cured. He said, “Laurie, you're done with lymphoma. Thanks to CAR-T, this cancer now has a cure.”
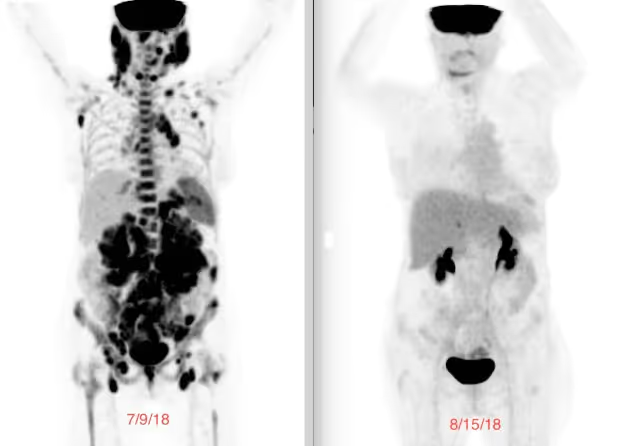
My little boy was my biggest motivator
I relapsed six times over the course of 12 years and was in continuous treatment all those years. People ask me, “Laurie, how did you do this? How did you keep going?” My motivator was my little boy. The thought of my husband having to tell my son that mommy died…it was just unfathomable. I said, I cannot let that happen. I have to fight. And if something doesn’t work, I have to find the next thing. I don't care what I have to do. I am not dying. My husband said, “What about me?” Of course I did not want to leave my husband either, but reminded him “You can get another wife, but our son cannot get another mom.”
Those 12 years felt like a roller coaster. Every time I would get optimistic, I’d get slammed down again. But I’d pick myself back up, brush myself off, and tell myself, “Find the next treatment, maybe it will work.” I vividly remember picking my son up from school when he was in the First Grade. I’d be waiting at the picnic bench when the class door would open and out he would run to me and jump into my arms. I’d say to myself, “I can’t miss these moments. I have to find the next treatment.”
I know I’m biased because I'm his mom, but my son was always caring and responsible. He worked multiple jobs starting at age 13. He delivered newspapers, had lemonade stands, and was a junior lifeguard and a skate guard at a local ice rink. Choosing a college was very tough for him: stay in LA or go away. We encouraged him to go away. It was hard for him after watching me fight my cancer, a cancer diagnosis impacts everyone in your life. So my son flew across the country to have his college experience. The summer I received CAR-T, he was certified as an EMT so could volunteer during his college years.
My husband and I have been together now for 30 years. During my cancer fight, I was strong and tried to keep my husband and my son out of everything as much as I could. My husband had a business to run, and I wanted him to focus on that while I dealt with the cancer. He used to say, "You're going to outlive me, you're so tuned in with all the medical details."

Swimming was my meditation
I found out early in my treatment that I needed to be active physically, mostly because I was a wreck emotionally. I was depressed and anxious. One day after a chemo treatment I said, "When I get home, I'm going to put on my tennis shoes, and I'm just going to walk to the end of the street." So I did that, and when I got back I thought, "That was really good." Not long after that, I started swimming. I had been taking my son to swim lessons at a local community college pool in Santa Monica. One day while he was in his lesson, I thought, "I'm going to go to the adult pool. I'm going to try to swim laps." I was still doing chemo and it was summer, so it was hot. Walking was hard because I’d get dizzy in the heat. So the pool seemed like a good alternative. I remember that first day I swam nearly 20 laps. It felt so great. It was slow - just like the walking - but it really helped me emotionally. I’ve never been able to meditate or do yoga. I’ve tried, but they’re just not for me. Lap swimming became my moving meditation.
I also went on an antidepressant. I felt like I needed to do everything I could to get my head working with my body. Day to day tasks at times were both physically and mentally challenging. I remember one time, a man walked up to me in the grocery store. I was wearing a scarf and he said “Oh, you must be doing chemo. How can you put that toxic stuff in your body, it will kill you! You just need a macrobiotic diet and you’ll be fine.” There was a woman in line, right in front of me, and she chimed in saying “Excuse me, what did you just say?” She reprimanded him. It turned out she was a survivor.
This experience has changed my life’s mission
Raising awareness of the game changing CAR-T immunotherapy and the benefit of clinical trials is my work now. People think of clinical trials from the scary stories of old. I was an early convert to clinical trials. Three of the seven treatments I had in my 12-year journey were clinical trials, and all three were provided at no cost to me. I learned quickly that clinical trials are often much smarter than standard of care therapies, they are more targeted and typically have fewer side effects. I’m a huge advocate for education around clinical trials.
There are access issues. Living in LA, I had access to multiple cancer centers for treatments and trials. During my 12-year journey, I was treated at four large cancer centers in Los Angeles. But many people are lucky if they have just one place in their state where they can access a trial. I’m trying to help change this. I work as a volunteer legislative advocate for the Leukemia & Lymphoma Society at both state and federal levels, to help make laws that require pharmaceutical companies to have more diversity in trials (racially, ethnically, geographically, and socioeconomically). I also work on advocating for patients and raising awareness of newer therapies, such as immunotherapies, which are more targeted. If you’re being treated at a community oncology center with an oncology generalist, they’re likely going to be doing what they’ve been doing for the past 30 years, which is chemo, transplant, and more chemo. They can’t possibly keep up to speed with all of the newer developments. I was an advocate for myself and I pushed and I pushed and I pushed. But not all patients can do that. Some aren’t equipped to be their own advocates due to language barriers, and some don’t have caregivers to help them. There are so many barriers, and because of that, we don’t have nearly enough diversity in clinical trials.
Cancer patients have such a tough road
I now spend about 20 hours a week as a cancer volunteer advocate for three different nonprofits. Helping others navigate their cancer journeys is something I am adept at. I’m also working on getting into good physical shape, although I had a set back with a broken hip. The softness of my bones is largely due to my 12 years of cancer treatments, which required me to have loads of steroids.
I have other fundraising plans, too, specifically for immunotherapies. Cancer patients have such a tough road as is, and then it’s worsened based on your financial situation and the quality of your health insurance and your geographic location. For such a wealthy society, it’s really sad how hard patients have to fight for access to medications. The barriers you can face with a life-threatening illness…it’s a real tragedy in our country.


They couldn’t believe what I had gone through
Through my advocacy work, I’ve had some amazing opportunities to meet scientists, including the guy who founded the CAR-T company that manufactured my treatment. I was able to thank him in person, and we filmed him for the documentary I’m working on. He said, "Laurie, if it wasn’t for patients like you who actually agreed to do this trial, we wouldn’t be here." And I said, "But I had no other option. I was dead otherwise. I had no choice." He replied, “I know, but you still went through a lot and without you, we wouldn't have learned how to handle side effects.” I also had the chance to share my story with hundreds of employees from his company. Many of them cried. "We never hear patient stories,” they said. They couldn’t believe what I had gone through.
Caregivers play an extremely important role for patients. They act as support for the patient and as liaison between the patient and the medical team. Often times, depending upon what treatment a patient is getting, the caregiver will be run ragged with 24/7 demands. Not going through the treatment themselves, it can be very challenging for them to witness what the patient is experiencing, and caregivers can feel intense emotional pressure without having the ability to affect a change in the patient’s outcome. I always encourage caregivers to take care of themselves, find time for self-care. Asking others to take a shift so the caregiver can get a break is very important. Oftentimes too, the caregiver doesn’t know as much about the treatments and potential side effects. Learning as much as they can is very helpful so they understand what the patient is experiencing. Also it can be helpful for the caregiver to speak to a patient advocate who can help them understand what the patient is experiencing, and that it is normal. The non-profit Leukemia & Lymphoma Society (lls.org) has a First Connection Program, where a newly diagnosed or relapsed blood cancer patient and their caregiver can be connected with a patient on the road ahead of them. I speak to numerous patients and their caregivers, to try to help them on their journeys. I very much enjoy this volunteer work.
Representation Matters
Increasing diversity in clinical trials builds trust, promotes health equity, and leads to more effective treatments and better outcomes (NEJM). But there is much work to be done - and barriers to break - to improve awareness and access for all people.
Do you know someone who is a member of a marginalized community who has participated in a clinical trial? If so, we’d love to meet them and share their story. We hope to represent the many faces of clinical trials through this project, and inspire others by shining a light on their experience.
They can contact us here.


